Alternatives for Arthritis
Table Of Contents
- Introduction
- Steroid Drugs for Arthritis
- Nonsteroidal Anti-Inflammatory Drugs
- NSAIDs and Cardiovascular Complications:
- Topical NSAIDs
- Antibiotics for Arthritis?
- Non-Drug Alternatives for Arthritis (Food Remedies)
- The Gin-Raisin Remedy
- Certo and Grape Juice
- Knox Gelatin
- Vinegar and Juice
- Pineapple (Bromelain)
- Non-Drug Alternatives for Arthritis (Herbs & Spices)
- Ashwagandha
- Boswellia
- Turmeric (Curcumin)
- Ginger
- Pycnogenol®
- Stinging Nettle
- Apitherapy (Bee Stings) for Arthritis
- Acupuncture for Arthritis
- Other Options
- MSM & SAMe
- In Conclusion
Introduction
Are You At Risk?
If you are lucky enough to reach 85 years of age you will have a 50% chance of developing symptoms of knee arthritis. Overweight? Your likelihood of having sore knees goes up to 66%.
Even if you are slim and middle aged, you may not be immune from joint pain. Over 30% of those between 45 and 64 have been diagnosed with arthritis.
Did grandpa, mom or Uncle Charlie complain about stiff joints, sore knuckles or achy knees? If so, your genes are working against you. The data suggest that people with a family history of OA have a 50% greater risk of also experiencing symptoms as they age.
Did you play rough contact sports as a kid? Repeated joint injuries or accidents can increase the likelihood that problems will develop later in life.
Reduce Your Risks:
Since we don’t know the causes of OA, we can only guess at minimizing risks. You can’t choose your parents, so you can’t escape your genes. You can, however, influence how they behave. We call that gene expression. Anything you can do to minimize inflammation and reduce wear and tear will be beneficial. So, here are our unscientific recommendations:
Keep weight under control. Exercise but avoid traumatic injuries. Swimming, walking, biking, tai chi, yoga, and reasonable running are all worth considering. Eat real food. Avoid processed food as much as possible. Stick with non-inflammatory fatty acids such as those found in extra virgin olive oil, almond oil, avocado oil, coconut oil and macadamia oil. Add anti-inflammatory spices to your food such as ginger, turmeric, cinnamon, cumin seeds, garlic, black pepper and cayenne.
If Your Joints Hurt, You Have Lots of Company!
According to the Centers for Disease Control and Prevention, one out of every three people over 65 years of age has osteoarthritis (OA). The CDC says that more than 52 million adults have “doctor-diagnosed arthritis.” This may greatly underestimate the total number of people affected, though. It has been estimated that over 20 million Americans suffer symptoms but have never been officially “diagnosed” by a doctor.
Aging baby boomers are discovering that they are not indestructible or immune to painful joints. Like their parents and grandparents before them, they too are developing aching ankles, knees, hips and backs. Arthritis could make retirement a lot less enjoyable for boomers who were planning on an active lifestyle once they hit 65. It’s hard to jog, hike, play tennis or swing a golf club if stuff hurts.
Joint replacement surgery has become a growth industry in the United States. According to the American Academy of Orthopaedic Surgeons, nearly 5 million Americans now have artificial knees and another 2.5 million have artificial hips. Between 2000 and 2010 hip replacements doubled. Interestingly, such surgery went up 205% in people between 45 and 54 years of age, suggesting that this is not purely a disease of senior citizens.
The Great OA Mystery:
What causes osteoarthritis? The conventional wisdom was that OA was an almost inevitable complication of accumulating birthdays. Daily wear-and-tear over 70 or 80 years was supposed to take a toll on joints by causing inflammation and degeneration.
There are some problems with that theory, however. For one thing, many people seem immune to joint pain even into their nineties. Others develop achy ankles, nasty knees and stiff backs before they hit 50.
If wear and tear were the culprits, then desk jockeys who spend hours a day sitting should be less likely to experience OA. Au contraire. A sedentary lifestyle may actually increase the risk for joint problems. The Arthritis Foundation points out that physical activity may be “one of the best ways to keep joints healthy in the first place.”
If OA is brought on by wear and tear then very long-distance runners should experience problems with ankles, knees and hips at a relatively early age. The data are surprisingly unconvincing. Although elite football and soccer players may indeed be at increased risk for OA, long-distance runners may not be. Many analyses show no association between osteoarthritis and running (British Journal of Sports Medicine, Sept. 28, 2016). One study even suggests that runners have less inflammation in their knees rather than more (European Journal of Applied Physiology, Dec. 2016).
We suspect that traumatic injuries to joints, like those experienced repeatedly by football players, do cause chronic inflammation and ultimately joint deterioration. Walking or even running do not appear to be injurious to joints. Staying fit and keeping weight under control are essential for good health and may also benefit joints.
As far as we can tell, researchers have not uncovered a clear cause of osteoarthritis. And they sure as heck have not come up with a cure. There are no magic medications that reverse joint deterioration and eliminate pain permanently.
Steroid Drugs for Arthritis
Double bind: n.
1. A psychological impasse created when contradictory demands are made of an individual so that no matter which directive is followed, the response will be construed as incorrect.
2. A situation in which a person must choose between equally unsatisfactory alternatives; a punishing and inescapable dilemma.
This definition from the American Heritage Dictionary of the English Language describes the quandary arthritis patients face with pain relievers.
Put another way, they are between a rock and a hard place! On the one hand they must cope with sometimes debilitating aches and pains. On the other, many of the drugs doctors prescribe can have serious side effects. Some may even make osteoarthritis worse in the long run.
Steroid Side Effects
- Fluid retention, edema
- Insomnia
- Irritability, nervousness, mood swings, mania and steroid psychosis
- Disorientation, confusion
- Hypertension
- Loss of potassium
- Headache
- Dizziness, vertigo
- Muscle weakness
- Blood sugar elevation (diabetes)
- Irregular menstrual cycles
- Swollen face
- Hair growth (including on the face)
- Itching, rash, hives
- Increased susceptibility to infection
- Weakened bones (osteopenia, osteoporosis, fractures)
- Tendon rupture
- Glaucoma
- Cataracts
- Ulcers
A long list of side effects often creates confusion. Brain fog takes over after five or six adverse reactions. Katy in Illinois shares her real-life experience:
“I have a terrible ‘moon face’ as a side effect of steroids. My face is huge, round and swollen. My eyes are nearly slits. I have the fat deposit across my neck just under my chin. The drug has made my stomach huge; I look 9 months pregnant.
“Steroids gave me severe diabetes. I got cataracts in both eyes such that I could not read or drive. I had surgery and lens replacement on both eyes. My bones are basically chalk now. I just started Fosamax to try to keep fractures away if it can. I have tremors in my hands that no longer go away even when the drugs are out of my system.”
Arthritis Drugs: Deal with the Devil?
Because health professionals do not really know what causes arthritis the best they can hope for is “control” of symptoms. The standard strategy is to reduce inflammation, diminish pain, slow damage to joint tissue and improve range of motion. Those are lofty goals, but doctors often employ some pretty scary drugs in their attempt to manage OA. Because people in pain are willing to do almost anything to ease their misery and resume normal activities, they may rely on drugs that have the potential to cause serious harm. It’s a classic drug double bind (see definition in the sidebar).
Corticosteroids:
If you turned back the clock to the 1950s, you would hear about a wonder drug called cortisone. It was used widely to relieve joint pain, especially for people suffering from rheumatoid arthritis. Patients loved “corticosteroids” because such drugs reduced inflammation and made it possible to function. People who couldn’t get out of bed without pain were able to reclaim their lives.
Many doctors loved cortisone-type drugs too. When they prescribed prednisone in the 1950s and 1960s they felt like heroes because patients were so grateful. Corticosteroids worked like magic to relieve a host of hard-to-treat conditions, from arthritis and allergies to asthma and atopic dermatitis. That’s because they have profound effects on a broad range of immunological and inflammatory actions in the body. There are few other drugs that can dampen inflammation and immune response so effectively.
In addition to cortisone and prednisone, doctors prescribe dexamethasone, hydrocortisone, methylprednisolone and prednisolone. If there is a “sone” at the end of the drug you can be fairly confident that the medication in question is a corticosteroid. These drugs can be incredibly helpful for some very serious health conditions including:
- Addison’s disease
- Life-threatening allergic reactions like anaphylactic shock
- Brain tumors or traumatic brain injury
- Inflammatory bowel diseases like Crohn’s
- Severe asthma uncontrolled by other means
- Autoimmune diseases like multiple sclerosis (MS)
For such serous conditions corticosteroids can literally be life savers. Some people have to take a drug like prednisone for long periods of time, if not indefinitely. These drugs must never be stopped suddenly. Doing so could trigger disastrous consequences. If a steroid needs to be discontinued, it must be under medical supervision!
The Dark Side of Corticosteroids:
As helpful as these drugs can be for people in dire straits, they pose some very serious complications when taken for long periods of time. In some circumstances the trade off is well worth it. In others, though, adverse reactions can be disastrous.
In addition to some of the very serious side effects listed in the sidebar, oral corticosteroids can cause acne, increased appetite and weight gain, high blood pressure, thin skin that bruises easily and impaired wound healing. There is also evidence that cortisone-like drugs are associated with the irregular heart rhythm called atrial fibrillation (Drugs, Aug. 20, 2012; JAMA Internal Medicine, May 8, 2006).
Psychological Side Effects:
A surprisingly common complication of corticosteroids involves neuropsychiatric reactions. Psychological side effects include irritability, depression, suicidal thoughts, anxiety, confusion and aggressiveness (American Journal of Psychiatry, May, 2012). Many patients are not warned about such problems when they get a prescription for prednisone or related drug. It’s hard to understand the impact of such adverse drug reactions until you visit our website. You will find hundreds of case reports at this link.
Here is a story from L. in Alabama:
“I was prescribed prednisone for a sinus infection (20 mg, two times a day for five days). The first three days I spent awake. The insomnia and night sweats allowed about 5 hours of sleep over three days. I was lightheaded, really depressed with suicidal thoughts and I was nauseated all day long. I had sudden increases in heart rate; I was incredibly angry and became delusional. Even after finishing the drug, I’m still having episodes of depression and nausea. I also have a nearly unbearable headache that is contributing to dizziness and face tingling. On top of all that, my face broke out in steroid acne. It’s red, swollen, inflamed, and hurts so bad.
“The headache I have now makes me really question my ability to drive. The side effects from prednisone are so so much worse than what I was dealing with before. At the follow-up, I told my doctor all the things I was dealing with now, and that I thought they were drug side effects. He scoffed and said ‘probably’ but didn’t say anything else.”
This story demonstrates that even a short course of steroid can produce dangerous adverse reactions. The higher the dose and the longer someone takes a drug like prednisone, the more likely there will be serious side effects. Make sure your physician is monitoring things like potassium, blood sugar, bone density and psychological well-being. And never stop a corticosteroid suddenly!
Nonsteroidal Anti-Inflammatory Drugs
| Generic | Brand |
| Celecoxib | Celebrex |
| Diclofenac | Cataflam, Voltaren |
| Etodolac | Lodine |
| Flurbiprofen | Ansaid |
| Ibuprofen | Advil, Motrin, etc. |
| Indomethacin | Indocin |
| Ketoprofen | Orudis |
| Meloxicam | Mobic |
| Nabumetone | Relafen |
| Naproxen | Aleve, Anaprox, Naprosyn |
| Piroxicam | Feldene |
| Sulindac | Clinoril |
NSAID Side Effects:
- High blood pressure
- Fluid retention, edema
- Heart attacks and strokes
- Irregular heart rhythms (atrial fibrillation)
- Congestive heart failure
- Digestive distress (indigestion, heartburn, ulcers)
- Perforation of the stomach, small intestine and large intestine
- Kidney damage, kidney disease
- Severe allergic reactions
- Toxic skin rash
- Stevens-Johnson syndrome
- Liver damage
- Blood disorders (anemia)
- Breathing difficulties (worsening asthma)
- Death
Unintended Consequences:
Kudzu, introduced to the US as an ornamental plant in 1876 and later used to prevent erosion in earthworks, has become a major problem in the southeastern United States. It often kills the trees it climbs on, and control is extremely difficult.
A Reader’s Experience:
“I was diagnosed with a stomach ulcer attributed to ibuprofen. I landed in the ER and almost died because I was taking Motrin.
“Every time I tell someone my story they are astonished. Most people are not aware that ibuprofen may cause stomach ulcers. They think stress, hot spicy foods or alcohol cause ulcers. So did I until it happened to me.
“Nothing on the back of the packaging warns that ibuprofen could cause dangerous internal bleeding. I want to warn other people to know so they won’t suffer as I did.”
Discounting Drug Side Effects
When someone experiences a heart attack or a stroke while taking an NSAID, it is not unusual for prescribers to blame the victim. We were once told by two drug company representatives that if someone died from an irregular heart rhythm while taking medication that the victim was most likely old and sick and would have died anyway. They implied the drug had nothing to do with the tragedy.
That attitude is a convenient scapegoat for all sorts of adverse drug reactions. Here is just one example from a visitor to our website.
“I was an otherwise extremely healthy woman when I suffered a mild stroke at age 53. I had been on a hiking trip and was taking ibuprofen several times a day for hiking-related muscle stiffness.
“Doctors have never been able to find the cause of the stroke despite numerous follow-up tests – my arteries are clear, etc. Looking back, I recall several times in the weeks before the stroke an occasional heart ‘flutter’ – as though my heart had an off beat. I can’t help but wonder if this wasn’t AFib and the cause of my stroke.
“I posed the question about the use of ibuprofen to my neurologist when I discovered a study that had similar conclusions, and he of course pooh-poohed it.”
How Good Are NSAIDs Anyway?
Despite the fact that NSAIDs have been around for decades and have been prescribed to tens of millions of people to relieve arthritis pain, there is surprisingly little evidence that they really do much good. Norwegian scientists searched the medical literature between 1966 and 2004 and discovered 268 randomized controlled trials of NSAIDs (BMJ Dec. 4, 2004). Many did not use a placebo control group. Others did not provide pain scale data. Ultimately, they analyzed 23 trials involving 10,845 patients (7,767 got NSAIDs and 3,078 received placebos). They reached the following conclusion:
“NSAIDs can reduce short term pain in osteoarthritis of the knee slightly better than placebo, but the current analysis does not support the long term use of these drugs…As use of oral NSAIDs may incur serious adverse effects, they can only be recommended for limited use in osteoarthritis of the knee.”
Osteoarthritis is Not Short Term
So here’s the rub: NSAIDs have been shown to work for a few weeks to ease the pain and inflammation of osteoarthritis. The trouble is that by definition OA is long-term. It does not go away after a few weeks.
Physicians believe in “evidence-based medicine.” That means they are only supposed to prescribe drugs that have been scientifically tested in randomized controlled trials. But the benefits of NSAIDs to treat OA for months or years remains untested.
Misperceptions About NSAIDs
Once physicians realized how dangerous corticosteroids could be, they became somewhat more cautious about how they treated arthritis patients. Aspirin became a drug of choice and large doses were frequently recommended, especially for people with rheumatoid arthritis. It was not unusual for a rheumatologist to recommend 14 or more aspirin pills a day.
In 1965 a new prescription medicine was launched. Indomethacin (Indocin) was seen as a potentially safer alternative for arthritis patients. It, like aspirin, belonged to a class of drugs called nonsteroidal anti-inflammatory drugs (NSAIDs). That word “nonsteroidal” gave the impression that these medications were substantially safer than steroids such as cortisone and prednisone. Patients were led to believe that NSAIDs wouldn’t cause the kind of serious complications associated with corticosteroids.
A survey of patients’ knowledge of adverse reactions to medications (British Journal of Clinical Pharmacology, Aug. 2006) confirms that this message was successfully communicated.
“Corticosteroids were ranked most dangerous by patients…Patients identified NSAIDs as low risk…In conclusion, patients’ knowledge of the risks associated with their medications is frequently inaccurate and at best inconsistent.”
Doctors embraced each new NSAID as it became available. When a different NSAID was launched with much fanfare, many prescribers lost enthusiasm for the old pain reliever and switched allegiance to the new anti-inflammatory agent that had captured the limelight. Drugs like Clinoril (sulindac), Feldene (piroxicam), Motrin (ibuprofen), Naprosyn (naproxen), Voltaren (diclofenac) and Mobic (meloxicam) were hugely popular in their day until replaced by something newer. NSAIDs became some of the most successful pharmaceuticals on the planet and are still widely prescribed for pain and inflammation.
For many physicians, nurse practitioners and physician assistants (PAs), NSAIDs remain their go-to pain relievers, especially now that opioids are under intense scrutiny by the DEA (Drug Enforcement Administration). The perception by many health professionals is that drugs like diclofenac, ibuprofen, meloxicam and naproxen are reasonably safe. The FDA considered NSAIDs so safe, in fact, that it allowed both ibuprofen (Advil, Motrin IB, etc) and naproxen (Aleve) to be switched to over-the-counter status.
On any given day, an estimated 20 million Americans swallow NSAIDs to ease a headache, soothe a sore joint or relieve the inflammation of tendonitis, bursitis or back pain. Many people never bother to read the instructions or warnings on OTC pain reliever labels. Even if they did, there is not a lot of information about the potentially life-threatening adverse reactions associated with NSAIDs. Many of the complications of these drugs have only been discovered over the last decade or so and serious side effects have seemingly not penetrated public awareness.
NSAIDs: A Double-Edged Sword
Nonsteroidal anti-inflammatory drugs work by blocking the body’s ability to make chemical messengers called prostaglandins (PGs). These hormone-like compounds have a profound impact on cells throughout the body. Sprain an ankle, hit your thumb with a hammer, have a tooth extracted or cope with osteoarthritis of the knee and chances are good you will experience inflammation. This can manifest as pain, redness and swelling due to activation of prostaglandins in your tissues. NSAIDs partially block the formation of prostaglandins by interfering with the enzymes responsible for their manufacture.
The trouble with NSAIDs is that they are not very selective. In addition to blocking inflammatory prostaglandins, they also block certain highly beneficial prostaglandins. Some of these compounds are essential for good health. They help prevent blood clots by making platelets less sticky. They dilate blood vessels and promote blood flow to the kidneys. PGs are crucial during labor and delivery. They also help protect the lining of the digestive tract by facilitating the formation of protective mucus.
By upsetting the body’s ability to make essential PGs along with inflammatory PGs, the natural homeostatic balance in the body can be seriously compromised. Think of NSAIDs a bit like herbicides, fungicides and pesticides.

A farmer can get rid of unwanted weeds, fungi and pests by spreading these chemicals on a field, but he can also kill helpful organisms. Upsetting the healthy balance of microorganisms in the soil and disrupting the harmony of nature can lead to unanticipated complications. Some herbicides and pesticides have endocrine disrupting activity and can alter the balance of hormones like estrogen and testosterone in various species. That can affect fertility and lead to birth defects in some animals. Killing beneficial insects (like bees) and certain plants can also change the balance of nature. There are also concerns that these chemicals may promote neurological changes and even cancer.
Prostaglandins and the GI Tract
Prostaglandins protect the stomach lining from damage. NSAIDs block prostaglandins in the digestive tract as an unintended consequence of their action. If you disrupt the production of the good prostaglandins with NSAIDs, you can produce classic GI symptoms such as nausea, indigestion, abdominal pain, constipation and/or diarrhea. It is estimated that over half of the people taking NSAIDs experience some of these complications.
Far worse, blocking beneficial PGs can lead to major GI damage. Many people end up with sores in their digestive tracts without any obvious warning symptoms. These lesions can become bleeding or perforated ulcers, which can be life threatening.
Experts have estimated that more than 100,000 people are hospitalized each year because of such complications, and more than 16,000 die (N. Engl. J. Med. 1999; 340:1888-1899). We suspect the numbers are much higher since so many people now take drugs like ibuprofen and naproxen without medical supervision.
NSAIDs and Cardiovascular Complications:
Once researchers had an inkling that Vioxx could increase the risk for heart attacks and strokes, they began looking at other NSAIDs as well. What they found over the last decade has shocked the medical community. They discovered that virtually all NSAIDs were capable of causing cardiovascular disasters. An FDA Public Health Advisory on April 7, 2005 warned: “NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction [heart attack], and stroke, which can be fatal.”
The FDA strengthened this warning on July 9, 2015:
“The risk of heart attack or stroke can occur as early as the first weeks of using an NSAID. The risk may increase with longer use of the NSAID.
“The risk appears greater at higher doses…
“NSAIDs can increase the risk of heart attack or stroke in patients with or without heart disease or risk factors for heart disease…
“There is an increased risk of heart failure with NSAID use.”
What Took So Long?
How is it possible that it took the FDA 50 years to recognize and warn about the really bad cardiovascular damage that NSAIDs can do? A high-level FDA executive shared with us his insights on this tragedy. He confessed that the agency is not very good at picking up common complications. In other words, lots of people take NSAIDs every day. Lots of people have heart attacks every day. Since the FDA was not looking for such an association, it did not connect the dots.
If a 63-year-old healthy woman suddenly died of a heart attack, her family and friends would mourn her premature passing. In such an instance it would be rare for anyone to ask if she had been taking an NSAID for a sore shoulder or a stiff knee. Even if someone asked that critical question, it is unlikely that her doctor would link her use of diclofenac or naproxen to the heart attack.
It turns out that it was easier for the safety sleuths at the agency to link NSAIDs to rare adverse drug reactions like kidney failure or bleeding ulcers than to heart attacks. As a result, many patients still do not appreciate the risks. After all, the FDA permits ibuprofen and naproxen to be sold over the counter. Most people assume that means they are totally safe.
The Latest Update on NSAIDs
Until recently, many health professionals clung to the hope that some NSAIDs might be safer for the heart than others. Because Celebrex (celecoxib) is in the same class of COX-2 inhibitors as Vioxx there was a hope that traditional NSAIDs like naproxen might be less less dangerous to the vascular system.
Steve Nissen, MD, is Chairman of the Department of Cardiovascular Medicine at the Cleveland Clinic. He is arguably one of the country’s foremost cardiologists. He and his colleagues conducted a large (24,000 arthritis patients) study of celecoxib, ibuprofen and naproxen (New England Journal of Medicine, Nov. 13, 2016). The “good” news was that celecoxib was no worse than ibuprofen or naproxen. The “bad” news was that it was no better than ibuprofen or naproxen. It turns out that all NSAIDs pose roughly the same risk to the heart and cardiovascular system. Dr. Nissen commented about the study:
“What is so surprising about it is that most authorities have believed that if there was a drug that was the safest, it was naproxen,” Nissen says. “So we were pretty surprised that there was this borderline significant increase in all-cause mortality with naproxen.”
Confirmatory Evidence
A meta-analysis of 280 studies involving 124,513 patients concluded that traditional NSAIDs like diclofenac and ibuprofen were just as dangerous to the heart as coxibs like Vioxx and Celebrex (Lancet, Aug. 31, 2013). The investigators concluded that the risk of heart failure was doubled whether people were taking traditional NSAIDs or the newer coxibs like Celebrex.
A study in the European Heart Journal (Oct. 4, 2016) followed 7,297 patients who were taking either Celebrex or traditional NSAIDs for roughly 3 years. They found that cardiovascular events were…”similar on celecoxib and NSAIDs.”
High Risk Patients Especially Vulnerable
People with high blood pressure or heart disease seem especially susceptible to NSAID nastiness. More than 22,000 volunteers from 14 different countries participated in a study that lasted over two years. Patients who used medications such as ibuprofen or naproxen were more likely to suffer heart attacks, strokes and death (American Journal of Medicine, July, 2011). The authors of the study concluded that, in patients with heart disease:
“chronic use of NSAIDs should be avoided where possible…Until further data are available, alternative modes of pain relief should be considered for these patients.”
People who have experienced heart attacks are in terrible trouble if they need a pain reliever. A Danish study of 99,187 patients who had experienced a myocardial infarction (MI, also known as a heart attack) were substantially more likely to have another heart attack or end up with a designation “coronary death” if they used an NSAID-type pain reliever (Circulation, Sept. 10, 2012).
Take Home Messages
All NSAIDs (except aspirin), including the newer generation coxibs, can be hard on the heart. Whether it is celecoxib (Celebrex), diclofenac, ibuprofen, meloxicam or naproxen, there is an increased risk for heart attacks and heart failure.
High blood pressure and an irregular heart rhythm called atrial fibrillation (AFib) have also been linked to NSAIDs (BMJ Open, April 8, 2014). As far as we can tell there is no one NSAID that appears safer for the heart and cardiovascular system than any other NSAID.
Add these cardiovascular risks to other adverse drug reactions such as ulcers and intestinal perforations, blood clots in veins (deep vein thrombosis or DVT), kidney damage, ringing in ears, liver damage and blood disorders and you have a class of medications that cause some serious health problems. These complications are especially relevant for older people who are the most likely to be suffering from osteoarthritis. In other words, the very people who are likely to have hypertension, heart disease, reduced kidney function and AFib are the very ones who are most likely to be taking NSAIDs for pain and stiffness. This is the worst kind of catch-22.
What About Aspirin?
There was a time when rheumatologists prescribed large doses of aspirin for people with both osteo and rheumatoid arthritis. That was before the NSAIDs became so popular. In truth, aspirin was the first nonsteroidal anti-inflammatory drug. Unlike other NSAIDs, however, it does not increase the risk for blood clots that can lead to heart attacks and strokes. If anything, aspirin reduces the risks for these thrombotic events. That is why cardiologists may prescribe aspirin to high risk heart patients. By the way, there is no evidence that other NSAIDs are any more effective than aspirin when it comes to relieving the pain and inflammation of arthritis. Aspirin is also one of the least expensive drugs in the pharmacy.
Despite the good news about aspirin, it is not without risk. Many people develop ulcers, including life-threatening bleeding ulcers. Older people may be especially vulnerable to this complication. Some people are allergic to aspirin or take drugs that are incompatible with it. No one should take aspirin regularly without medical supervision. There are, however, some relatively old drugs that can provide pain relief like aspirin does, without the digestive dangers.
Alternatives to Aspirin
There are two little known aspirin-like drugs that have been around for years. Both are less likely to irritate the stomach than aspirin. We suspect that relatively few health professionals or patients are aware of salsalate (salicylic acid). This drug has been around for more than a century. And yes, it is closely related to aspirin (acetylsalicylic acid). What makes salsalate intriguing is its powerful anti-inflammatory activity. It helps ease symptoms of osteo or rheumatoid arthritis but is less likely to cause stomach irritation or ulceration compared to aspirin or other NSAIDs.
Other Salsalate Benefits
Because salsalate has been around so long it has received relatively little attention. There is new research, however, that suggests this very old medicine might have a very bright future. It blocks a key inflammatory pathway involving something called NF-kB (nuclear factor-kappa B). This protein complex affects almost every cell in your body. When NF-kB is inappropriately activated it appears to play a key role in cancer, inflammation, brain function and immunity. Drugs, herbs, spices and dietary supplements that block NF-kB may have potent anticancer and anti-inflammatory activity. That’s where salsalate enters center stage.
Scientists suspected that salsalate might be helpful against diabetes as far back as 1876. Recent research has confirmed that the drug can help control blood sugar and may be beneficial against prediabetes. In addition it appears to lower blood pressure, triglycerides, LDL cholesterol and other inflammatory markers “with minimal side effects” (American Health & Drug Benefits, June, 2014). The authors of this article conclude:
“This medication, which costs pennies a day, could be a useful and cost-efficient option in the treatment of individuals with prediabetes and the prevention of progression to diabetes.”
Preliminary research in animals suggests that salsalate may also be beneficial against dementia by blocking the buildup of a toxic brain protein called tau (Nature Medicine, Oct., 2015). There is also a possibility that salsalate might enhance cancer treatment (both chemo and radiation therapy) by reducing NF-kB activity, which is often elevated in cancer cells (Integrative Cancer Therapy, Sept, 2006).
Side effects of salsalate include tinnitus (ringing in the ears), dizziness, rash, itching, nausea, altered kidney function (increased serum creatinine and albumin) and atrial arrhythmias. That said, the authors of a controlled trial note that, “Overall, there were no clinically meaningful differences in serious and nonserious adverse events between the salsalate and placebo treatment arms” (JAMA Cardiology, July, 2016). Salsalate is available only by prescription as Amigesic, Artha-G, Disalcid, Mono-Gesic and Salflex. It is unlikely to prevent blood clots the way aspirin does.
Choline magnesium trisalicylate (Trilasate, Tricosal, Trisalicylate) may also be a little less likey to upset the stomach than aspirin. Like salsalate, this pain reliever won’t protect against heart attacks or strokes the way aspirin does. It also requires a prescription.
Topical NSAIDs
Reader Stories Re: Topical NSAIDs
Whitley in North Carolina reports:
“I started applying Voltaren Gel in 2007. I use it on my knees when I have an active period ahead. I get 5-6 hours of excellent pain relief from Voltaren Gel. Two doctors have told me that some NSAID will reach your blood but not in large enough amounts to worry about.
“I recently injured a rotator cuff and Voltaren Gel works very well on the shoulder. After 9 years I’ve had zero negative reactions.
“As to reading side effects on the bottle – lawyers have made those lists so long my eyes glaze over. I read the main problems to look out for. Voltaren Gel works for me.”
Joan in Edmonds, Washington:
“My husband and I have been using Voltaren Gel for years. I am bone on bone on both knees and feel that without Voltaren, I would not be able to walk. I put a small amount on my knees in the morning and then get on with life. My husband has some serious back issues so he puts Voltaren Gel on at night. At 84 he is able to function quite well, including gardening, mowing the lawn, etc.
“Voltaren Gel is OTC in Canada so we cross the border several times a year to replenish our supply. No problem bringing it back into the US. No adverse reactions.”
Errol in Donalds, SC warns about side effects:
“I quit taking oral NSAIDs several years as my doctor advised because of early stage kidney disease. After a bad knee injury a specialist put me on Voltaren gel for 9 months. Now I am in stage 4 kidney disease. I had been stable for several years before the daily use of Voltaren gel.”
We have found the FDA’s behavior with regard to NSAIDs bizarre. On the one hand, the agency has allowed drugs like ibuprofen and naproxen to be sold over the counter despite the growing recognition that such drugs can cause hypertension, atrial fibrillation, heart attacks, strokes, perforated ulcers and heart failure, to name just a few serious adverse reactions.
On the other hand, the FDA was very slow to allow patients access to topical NSAIDs in the forms of creams and gels. This, despite the fact that such drugs have been available around the world for decades. Many countries allow these topical NSAIDs be sold without a prescription. In the U.S. the FDA finally approved the gel form, Voltaren Arthritis Pain, for OTC sale in February, 2020. The active ingredient diclofenac is also available by prescription as Pennsaid Topical Solution. Another form of topical diclofenac is the Flector® patch, with 1.3% diclofenac epolamine. Whereas physicians in Australia, Canada and Italy are likely to recommend such products to patients with osteoarthritis, American physicians are far more likely to prescribe oral NSAIDs.
Are Topical NSAIDs Safer?
A question we get asked repeatedly is whether products like Voltaren Gel are as hazardous as oral diclofenac, ibuprofen or naproxen. The answer depends upon who you believe. The Food and Drug Administration is extremely cautious about topical NSAIDs. Here is the black box warning you will find on Voltaren Gel. It is not that different from the warning you find on oral diclofenac:
“Non steroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction [heart attack] and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use.
“NSAIDs can cause an increased risk of serious gastrointestinal (GI) adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms.”
In essence, the FDA believes that whether you apply the medication to your knee as a gel or swallow a pill, the risk is the same. Other experts disagree. A review of the research on topical ketoprofen gel found that it was better than oral celecoxib or placebo for treating symptoms of knee osteoarthritis with fewer adverse events (Musculoskeletal Care, Oct. 24, 2016). Skin irritation was the most common side effect.
The Cochrane Collaboration vs. the FDA:
The Cochrane collaboration is an independent and highly respected non-governmental organization that evaluates the benefits and risks of pharmaceuticals and other treatments. It reviewed 61 studies of topical NSAIDs and concluded:
“Topical NSAIDs provided good levels of pain relief in acute conditions such as sprains, strains and overuse injuries, probably similar to that provided by oral NSAIDs. Gel formulations of diclofenac (as Emugel), ibuprofen, and ketoprofen, and some diclofenac patches, provided the best effects. Adverse events were usually minimal.” (Cochrane Database of Systematic Reviews, June 15, 2016).
We tend to trust the independent Cochrane analysis more than the FDA’s standard NSAID labeling. That’s because the Cochrane authors constantly review the medical literature and revise their publications when new research becomes available. The FDA often moves slowly to update its labeling. That said, some people are so sensitive to NSAIDs that even a topical formulation may cause problems.
Antibiotics for Arthritis?
This sounds bizarre, right? Why would anyone consider taking a tetracycline-type antibiotic like doxycycline to ease joint pain? You might be surprised to learn that there is evidence that doxycycline might be helpful for treating osteoarthritis as dating back to the early 1990s (Journal of Rheumatology, Oct. 1991).
In 2005 a study demonstrated that doxycycline might slow joint damage in the knee (Arthritis & Rheumatism, July, 2005). This was a multi-center research effort. Rheumatologists recruited 431 overweight women between the ages of 45 and 64. The volunteers were randomly assigned to receive either a placebo or 100 mg of doxy twice a day for 30 months. That is a long time for a clinical trial.
The investigators were looking for a measurable outcome and opted for joint space narrowing in the knee. The authors concluded:
“Doxycycline slowed the rate of JSN [joint space narrowing] in knees with established OA [osteoarthritis].”
Specifically, the group taking doxy had 40% less narrowing than the group on placebo at 16 months and 33% less narrowing after 30 months. Joint pain was low in both groups but the group taking the antibiotic were less likely to see a worsening of their pain over previous visits.
How does an antibiotic like doxycycline make a difference in osteoarthritis? When most people think about antibiotics they think antibacterial activity. Doxy is prescribed for Lyme disease, Rocky Mountain Spotted Fever, bacterial pneumonia and many other infections. But doxycycline has other mechanisms of action. In the case of osteoarthritis it appears to to be a DMOAD (disease-modifying osteoarthritis drug).
There are several mechanisms and we won’t bore you with the molecular details. There is, however, evidence that this antibiotic inhibits collagen breakdown (Journal of Clinical Medicine, April 18, 2023). By reducing the breakdown of cartilage, it can slow the degeneration of joint tissue linked to osteoarthritis.
Would we recommend doxycycline as a primary treatment for osteoarthritis. No. That’s because it can disrupt the microbiome of the digestive tract. Digestive upset and diarrhea are relatively common side effects. It also makes the skin more sensitive to ultraviolet radiation from the sun. There are other adverse reactions, though they are less common.
All that said, dermatologists have been prescribing doxycycline to teenagers for decades to treat acne. While doxy’s side effects are of concern, so are the complications of nonsteroidal anti-inflammatory drugs. It would be great if the NIH funded long-term clinical trials to assess the effectiveness of this antibiotic for osteoarthritis and compare it to NSAIDs like like ibuprofen or naproxen.
How Effective Are FDA-Approved Arthritis Drugs?
Despite enthusiasm for FDA-sanctioned medications, remember that NSAIDS are not all that effective.
Norwegian researchers writing in the BMJ (Dec 4, 2004) concluded that:
“The advantage of oral NSAIDs over placebo for short term pain relief is small and probably clinically insignificant. Evidence of long term effects from oral NSAIDs is still lacking.”
In one study published in the New England Journal of Medicine (Nov. 13, 2016), over 24,000 subjects were assigned to take either celecoxib (Celebrex), ibuprofen or naproxen for roughly 20 months. The drop out rate was astounding. By the end of this clinical trial 16,658 people gave up on the program. That’s a whopping 69%. Presumably these arthritis patients were given free medicine. The fact that more than two-thirds said no thanks suggests that none of these NSAIDs worked that well to control their arthritis pain and inflammation.
Non-Drug Alternatives for Arthritis (Food Remedies)
Cherries: Life Is Just a Bowl of Tart Cherries (Reader Stories):
“I have suffered from arthritis in my right hip for several years. By last fall it got so bad I could hardly walk. Over the years, I tried lots of supplements for joint health advertised on TV. I have also had two expensive injections into my hip that gave me relief for only a few days. Nothing was helping.
“I was unable to exercise and was having a very difficult time doing my job. My X-rays looked horrible and the surgeon who will do my hip replacement wondered how I was even walking.
“I don’t remember when I heard about cherries, but I started eating Bing cherries in the spring. I also started drinking tart cherry juice concentrate mixed in water. I finally got some real relief!
“It has been a very effective anti-inflammatory for me. I can climb stairs, exercise, mow the grass, and work without a lot of pain. These are things I have not been able to do for a few years. I will still have hip surgery next summer, but until then, tart cherry juice is the best!”
Gout or Arthritis:
“At 39, my brother had knots come up on his shins, and swelling in ankles and knees, along with pain so excruciating he could barely walk. He had labs drawn and his uric acid levels were extremely high. The doctor diagnosed it as gout.
“My brother couldn’t afford the traditional medicines, so he took pure cherry extract. Within three days, the knots and pain disappeared and his uric acid had come down to normal when he had new labs drawn the next week. He has had no problems since.
“His doctor agreed that the cherry juice must have been effective since he had no other treatment. I have used cherry extract successfully for joint pain as well.”
Q. I was on Celebrex but had side effects. A friend recommended that I try Brownwood Acres tart cherry juice. It took four weeks to kick in, but at the ripe old age of 79 I’m tap dancing again. It worked for me.
A. We’ve heard from others that tart or sour cherries or cherry juice might ease joint pain from gout. Your testimonial is terrific, and we suspect others will want to try cherry juice for arthritis as well. The brand you mention is available at www.brownwoodacres.com or (877) 591-3101.
The research protocol in one study mentioned a dose of two 8-ounce bottles of tart cherry juice daily. Some readers find Montmorency cherry juice concentrate is more economical.
If an herb or dietary supplement caused a fraction of the side effects of oral over-the-counter or prescription arthritis drugs, the FDA and the medical establishment would have gone on the warpath and banned it decades ago. Imagine if someone reported that aloe vera juice raised blood pressure or harmed the kidneys. The media would be all over the story and headline writers would have a field day. The FDA and most health professionals would immediately call for a ban on aloe vera. The public would be warned about the dangers of home remedies and encouraged to stick with FDA-approved drugs.
Natural remedies that have anti-inflammatory activity are pretty much ignored by mainstream medicine while corticosteroids and NSAIDs are prescribed by the boatload. We have heard surprisingly few concerns raised about the side effects of NSAIDs such as hypertension, heart attacks, strokes, atrial fibrillation, heart failure, kidney damage, liver damage, intestinal ulceration and perforation. There are no calls to ban OTC ibuprofen or naproxen or limit the use of such drugs despite the many grave consequences of regular use.
Perhaps it’s time to consider some natural approaches to controlling arthritis symptoms. There is an impressive amount of scientific support for the anti-inflammatory action of culinary herbs and spices. Home remedies for arthritis may not have double-blind, placebo-controlled trials to support their effectiveness, but many people find them helpful and they certainly do not carry the risks of corticosteroids and NSAIDs. And remember that FDA-approved drugs have not been proved to be all that effective for arthritis when taken for long periods of time.

Cherries for Arthritis & Gout
Ask a health professional about nondrug options for pain and inflammation and you are likely to get a blank stare. Medical students are not taught about tart cherries. But there is a surprising amount of science to support this botanical approach.
We first heard about the anti-inflammatory power of cherries in 1999 from a reader of our syndicated newspaper column.
He said tart cherries could ease a gout attack:
“I eat five tart canned cherries a day to prevent gout. If I feel an attack coming on I eat 20 or 30 cherries and it is usually gone the next day. I have not had to take any pills for gout for six years.”
Since then we have heard from countless readers and visitors to our website that tart (or even sweet) cherries have healing properties, and not just against gout.
“I have been taking the tart cherry juice for about 14 years now and I wouldn’t be without it. The syrup [diluted in water] is the best way to take it.
“I have very little arthritis pain as long as I swallow the cherry juice on a regular basis. When I don’t take it, my hands ache so much I can’t sleep. I started with a tablespoon and have progressed to 2 tablespoons as I have gotten older.
“I am in good health and only take blood pressure medications and lemon flavored cod liver oil. I have ordered my cherry juice on the internet from northern Michigan for years. I am 73 years old.”
It turns out that cherries contain anthocyanin compounds that inhibit enzymes called COX-1 and COX-2 (Phytomedicine, Sept., 2001). These enzymes are the same ones that are inhibited by anti-inflammatory drugs like celecoxib, diclofenac, ibuprofen and naproxen. As far as we can tell, cherries do not cause stomach ulcers, raise blood pressure or cause heart attacks and strokes. So ingredients in cherries affect the very enzymes responsible for pain and inflammation in a way that is comparable to FDA-approved drugs, but without the adverse effects.
There is evidence that cherry juice helps alleviate pain (Behavioural Brain Research, Aug. 12, 2004). It also lowers uric acid levels, one of the key ways physicians prevent or treat gout attacks (Malaysian Journal of Nutrition, Mar., 2009). One study involving 633 gout patients concluded that “cherry intake is associated with a lower risk of gout attacks” (Arthritis and Rheumatism, Dec. 2012).
There is a substantial amount of good research to suggest that tart cherries prevent symptoms of exercise-induced muscle damage in athletes (British Journal of Sports Medicine, Aug., 2006; Journal of the International Society of Sports Nutrition, May 26, 2016; Nutrients, July, 2016). We were especially impressed with a study carried out on horses (American Journal of Veterinary Research, June, 2009). This double-blind crossover trial randomly assigned horses to either a tart cherry juice blend [TCJB] prior to exercise or a placebo solution. Measurements of muscle breakdown and inflammation were analyzed. The tart cherries reduced levels of aspartate aminotransferase, an indicator of muscle damage.
The authors concluded that:
“Administration of TCJB may diminish muscle damage induced by exercise.”
Since neither the horses nor the handlers knew when the tart cherry juice or placebo were being administered, we are reasonably convinced that there is something in cherries that counteracts the impact of intense exercise on muscle tissue.
Although there are not a lot of randomized controlled trials of tart cherry juice in humans, we did find such a study published in the journal Osteoarthritis and Cartilage (Aug. 2013). Patients with knee arthritis were randomly assigned to tart cherry juice or placebo. The cherries lowered CRP (C-reactive protein) levels, a measure of inflammation. Patients also reported improved WOMAC scores (an arthritis questionnaire that assesses overall pain and stiffness as well as joint functionality).
The Gin-Raisin Remedy
Instructions for Preparing Gin & Raisins
A reader of our newspaper column sent us this clipping more than 20 years ago:
Raisin Recipe
“Empty one box of golden light raisins into a large shallow container. Pour enough gin to completely cover the raisins. Let stand, uncovered, for about seven days until all of the liquid evaporates. Stirring occasionally will help the evaporation process. After the gin has evaporated, place the raisins in a closed container …
“Eat nine raisins a day. If you don’t like raisins, put them on your cereal or in a salad.”
Attributed to “The Acts of Saint Lucas,” the newsletter of St. Lucas Lutheran Church, Toledo, OH.
FAQs (Frequently Asked Questions):
How long does it take for the gin to evaporate?
It depends a bit on the humidity in the air. It may take just a day or two, or it can take up to 10 days. The raisins will not be dry, but there will be no gin puddled in the dish.
Once the raisins are ready, should they be refrigerated?
They should be kept in a tightly covered container. Refrigeration will extend the shelf life.
How much alcohol is in the raisins?
There is approximately one drop in the daily dose of nine raisins.
Does it matter what type of gin?
You don’t need to buy the most expensive gin, since you will let it evaporate. Don’t buy the cheapest one, either. Ask the clerk to help you find a gin that is flavored with real juniper berries rather than artificial flavorings. Some people report using sloe gin. Sloe gin is flavored with blackthorn berries rather than juniper. Blackthorn berries were traditionally used for digestive problems but might have some anti-inflammatory properties. Other people have substituted vodka or rum.
Do I have to use gin? I do not drink any alcoholic beverages!
Some people cannot stand the taste of gin. Others never consume alcohol, even if nine raisins only contain one drop of alcohol. Some people report success using vinegar in place of gin: “I combine 2 parts apple cider vinegar and 1 part honey (which kills the taste of the vinegar). Add this liquid to a box of golden raisins till just covered. Soak for three days and eat 9 raisins a day.”
Can you use dark raisins?
Some people do. Most people prefer the golden raisins. Others report using dried apricots. One variant, soaking dark raisins in sloe gin, results in a very dark purplish concoction. But if it helps ease aches, color should not be a problem.
Are there any side effects?
People who are sensitive to sulfites must avoid golden raisins, since they are treated with sulfites. Sticking to nine raisins daily should reduce any digestive tract issues such as gas.
Will I flunk a Breathalyzer test after eating the raisins?
Don’t keep the raisins in your vehicle. Take them at least half an hour before you might be tested. A Breathalyzer might be able to pick up traces of alcohol within a few minutes of eating the raisins.
WHY THE HECK IS IT 9 RAISINS?!?
I mean, 10 is a nice round number… would 10 raisins (or 12 or 15) really be a deal breaker? Yes they are delicious… so I do eat about 15 per day. As far as I know, they do work.
I just found out recently that my kneecap is severely off to one side and has been that way for 2-3 years. Still, I ski the double-diamonds hard, at 68, and have just a little pain. I was just told I should have a LOT of pain doing that, but I don’t. Probably it’s because of those raisins. Cheers!
We wish we had an answer for Cindy (the person who asked above about why 9 raisins). Someone suggested that 9 is a magic number. That may be, but a lot of folks just eat a spoonful and don’t worry about counting out 9 raisins. Since this is a home remedy, there are no studies to answer this frequently asked question.
More Stories from Readers
Lloyd in Texas was in real pain:
“I am a 64-year-old man. I started experiencing a lot of pain in my hands. I assume it is arthritis. It became so painful that I was afraid to shake hands. I bought a bottle of organic Prairie Gin. I added this to the dark raisins I had on hand.
“Within three days, I noticed a substantial improvement. One week later my pain was about 80% gone. The next batch I made was with golden raisins. Possibly the golden raisins are better. I will continue to experiment.
“I eat a spoonful of raisins every day. If I miss a couple of days, my pain returns. What a great remedy.”

The “Gin-Raisin Remedy”
We first heard about eating nine gin-soaked raisins for arthritis more than 27 years ago. On May 16, 1994 we received this letter:
“A neighbor gave my wife a recipe for ‘arthritis relief’ that involves soaking golden raisins in gin. When the gin has completely evaporated she is to eat nine raisins a day.
“She’s just starting to eat these raisins, so we don’t know yet whether it will make any difference. Our neighbor says it has helped his shoulder pain. What do you think?”
We were amused and more than a bit puzzled by this arthritis remedy. First, it made no sense to us. Why nine raisins? Why golden raisins? And what did gin have to do with arthritis relief? We decided to include this message in our newspaper column in large measure because it was one of the most original home remedies we have ever received to ease the aches and pains of arthritis. We speculated that the juniper flavoring in gin might have something to do with the purported benefits. There was certainly nothing in the medical literature to support this odd concoction.
It wasn’t long before we started hearing from readers who either had long experience with this home remedy or who tried it and liked it. Over the last two decades, we have heard from hundreds, if not thousands, of readers that the gin and raisin remedy was helpful. Not everyone reports success, but we are constantly surprised and delighted by the number of people who do. Here is a recent question along with our answer:
Q. I stopped taking glucosamine in favor of gin-soaked raisins with terrific results. I’m a former runner with serious but not debilitating knee and hip pain. When I read about gin-soaked raisins I thought it sounded silly.
I gave it a try anyway. It worked. I haven’t used the pills now for over eight months.
I’m curious: why golden raisins? Sometimes golden raisins are not readily available. Will plain old black raisins work just as well? I like to know why something works.
A. We’ve been searching for research on gin-soaked raisins for joint pain for years. Sadly, home remedies are rarely studied in randomized controlled trials. As a result, we don’t have a good answer to your question.
There are data to suggest that grape juice may have a number of health benefits. They include enhanced performance and reduced inflammation in runners (Applied Physiology, Nutrition, and Metabolism, Sept. 2015). Grape juice also appears to make blood vessels more flexible and improve cognitive performance (Nutrients, Dec. 2, 2015; American Journal of Clinical Nutrition, March, 2016). Since raisins are dried grapes, this might help to explain why so many people find the raisin remedy helpful.
A study in rats showed that the compounds in grape seed help protect against joint damage (Experimental & Molecular Medicine, Oct. , 2011).
Dion in New Zealand (the remedy has spread) shared this success story:
“I am 69 years old and have been getting leg pain for the past three or four years, especially when I try getting up from sitting for a while. I was putting this down to my daily workouts at the gym. Then I went on holiday for three weeks, and the pain only got worse. I was having trouble walking and getting bad cramps at night so the idea of the pain being related to gym exercise was false.
“Then I read about the gin and raisin remedy and have been trying that for about two months. WOW! What a change.
“I’m not getting any pain in my legs now and look forward to taking our dog for a walk up to three times a day. I soak the raisins in gin for about a week prior to taking them. I always have two containers on the go: one soaking while I use the other one.
“I have not noticed any difference between using white (golden) or black raisins and have used both as a trial. Give it a try. You have nothing to lose.”
Sophia got an unexpected bonus when she tried the gin-soaked raisins:
“I tried gin-soaked raisins for osteoarthritis, not expecting much, if anything. To my great surprise, my knee which had been badly swollen for several years, became almost normal sized within a few days.
“An even greater surprise was my breast, which had been greatly swollen from radiation damage a year ago, was reduced to normal. I didn’t know that gin-soaked raisins could reduce inflammation!
“When I stopped eating them, the inflammation returned. I bought another brand of gin but it didn’t work as before. My son did some research, and found that the gin should contain wild juniper. Check the label for that ingredient.
“Now I’m back on track, and am grateful to you for the surprising remedy. And the four pound weight loss was welcome!”
Another reader shared this experience:
“I am completely convinced that taking a teaspoon a day of gin-soaked raisins has done what the chiropractor could not do for my feet and ankles.
“I have a gardening business and MUST walk, shovel, rake and move around on uneven ground. I was in such pain it was becoming difficult to work, but this is my only source of income. Ibuprofen didn’t really help, but the raisins turned the condition around.”
Want to see how to make the gin-soaked raisins? Here is a short video:
Many health professionals have scoffed at the raisin remedy. They assume that if people get benefit it must be a placebo response.
They could be right, but here is a story from Darlene, a strong skeptic:
“I didn’t believe this remedy would work, so it was not the power of positive thinking! I don’t let the raisins dry out and I don’t count them. I just eat a spoonful every day, and it has been remarkable. Such a simple thing to do for a lot of relief. I have even commended it to a lot of people.”
Certo and Grape Juice
Can Pectin Provide Pain Relief?
March 30, 1998
Q. My wife and I tried your golden raisins and gin for arthritis and we were unimpressed.
We have discovered something else, though, that seems to work for us. Take two teaspoons of Certo dissolved in three ounces of grape juice. Do this three times a day. We have been told to cut back to one teaspoon Certo in grape juice twice a day after the joints quit aching.
We buy Certo in the grocery store near the canning jars. It’s simple and cheap and seems to be helping. I am on Coumadin so I can’t take anti-inflammatory drugs like Advil or Aleve.
A. Certo contains pectin, a natural ingredient found in the cell walls of plants. It is used as a thickening agent in jams, jellies and puddings.
Grapefruit pectin has been used to lower cholesterol, but this is the first we’ve heard of using pectin for arthritis pain. It seems safe, though we could find no scientific evidence to suggest it is effective for arthritis.
Since writing that newspaper column in 1998 there has been substantially more research into the health benefits of both pectin and grape juice (see studies to your right). We have also received hundreds of anecdotal reports of success.
Q. Thank you for writing about Certo and grape juice. I was having excruciating pain in the metatarsal area of my foot, which caused me great difficulty walking.
After two weeks of using Certo and grape juice as you described, my feet are free of pain. Why isn’t this remedy better studied and more widely known?
A. So far as we know, no research has been done to determine the effectiveness of purple grape juice and Certo (plant pectin used for making jelly) for joint pain. This remedy goes back at least to the 1940s, and we have heard from many people like you who have had success with it:
“My hands used to be stiff when I’d get up in the morning so I tried the Certo and grape juice. It worked wonders. I have been using it for over a month with better results than all the pills I was taking.”
FAQs re: Certo & Grape Juice:
What are the various recipes for this remedy?
There are a number of formulas. Since this is a home remedy, there is no science to support one recipe over another. Here are the most popular concoctions:
- 2 teaspoons of Certo in 3 ounces of grape juice (three times daily)
- 1 tablespoon Certo in 8 ounces of grape juice (once daily)
Grape juice is full of sugar. Is there any way to avoid this problem?
It is possible to find low-sugar grape juice. One reader, Celeste, offered this:
“If you have a Fred Meyer nearby, they have it in their health foods section. Another alternative is to ask your local grocery to bring in R.W. Knudsen ‘Just Concord’, if you want organic, pure no-sugar-added juice with no additives.”
Will this remedy interact with my medications?
Barbara answered this question for us:
“According to WebMD under Pectin interactions: ‘Pectin can affect how certain medications are absorbed including antibiotics and lovastatin. To avoid this take meds one hour before or four hours after taking pectin.’ I hope this helps others as it has helped me.”
Will the Certo and grape juice mixture create benzene?
Liquid Certo contains sodium benzoate as a preservative. Several websites warn that if it is mixed with citric acid, it will form the cancer-causing substance benzene. When we dug into this concern we discovered that a great many foods and beverages rely on sodium benzoate as a preservative. When there is vitamin C in the food or beverage it is conceivable that benzene would be formed, but are the levels high enough to worry about? When the FDA tested a variety of drinks for benzene, it found that levels were considerably below those considered hazardous.
We think that if you mix up a batch each time and drink it immediately, the benzene risk would be minimal. If you want to avoid sodium benzoate altogether, it is possible to get powdered pectin. Readers tell us that Pomona’s Universal Pectin, made from citrus fruit peel, contains no sugar, preservatives or additives. It is harder to get it into solution with grape juice, however.

Certo and Grape Juice
Not everyone benefits from gin-soaked raisins. Decades ago we received a question from a reader of our syndicated newspaper column. You can read the original question and answer in the sidebar to your left.
Since that original message in 1998 we have heard from hundreds of people who have used variations on this remedy with great success. Perhaps the grapes are just as important as the gin in gin-soaked raisins. There is actually a decent amount of research suggesting that ingredients in grape juice have anti-inflammatory properties (Arteriosclerosis, Thrombosis and Vascular Biology, Nov., 2004); American Journal of Clinical Nutrition, July, 2006).
In one study, the authors summarized their findings:
“In conclusion, dietary supplementation with concentrated RGJ [red grape juice] exerts hypolipidemic [cholesterol-lowering], antioxidant, and antiinflammatory actions in both healthy subjects and patients with end-stage renal disease. This effect may be considered to be beneficial for the prevention of cardiovascular disease.”
Not only did red grape juice lower bad LDL cholesterol, it raised good HDL cholesterol. Grape juice also lowered markers of systemic inflammation, which would be desirable for people with arthritis.
Researchers have also reported that Concord grape juice “improves memory function in older adults with mild cognitive impairment” (British Journal of Nutrition, March, 2010). It’s not just old folks who seem to benefit.
Another group of investigators reported in the highly regarded American Journal of Clinical Nutrition (March, 2016) that:
“consumption of CGJ [Concord grape juice] for 12 wk was associated with better spatial memory and safer driving behavior relative to placebo in this sample of healthy working mothers (aged 40-50 y) of preteen children.”
If grape juice is good for the vascular system and the brain, the same anti-inflammatory activity is likely good for the joints as well. That’s not idle speculation. Researchers have found that grape juice actually does exert anti-inflammatory activity at the cellular level. Both COX-2 and TNF [tissue necrosis factor] levels are decreased (Environmental Toxicology and Pharmacology, March, 2014). These are markers of inflammation that directly affect joints. Some of our most expensive arthritis drugs are specifically designed to lower COX-2 and TNF.
What Is the Story on Certo?
Plant pectin also appears to have anti-inflammatory properties. Like grape juice, it can modulate COX-2 expression (Biochemical Pharmacology, Oct 16, 2006). There is solid scientific evidence that pectin has numerous health benefits. It lowers cholesterol and other blood fats, improves insulin sensitivity and blood sugar control, enhances the diversity of good bacteria in the digestive tract and may reduce the risk of some cancers (Nutrients, June, 2015). Combining plant pectin with purple grape juice seems like a delightful way to enhance overall health.
It may account for some of the amazing stories we have received from readers.
“My purpose in writing is to share my extraordinary results as an encouragement for you to keep spreading the word so others might benefit. I am now sixty years old. I have had no cartilage in my right knee since 1967. Over twenty five years ago my osteoarthritis was confirmed by x-ray. I have had a very active life style: running over 30,000 miles, playing basketball (twice weekly for 40 years) and walking one to three miles daily.
“In the last several years my osteoarthritis symptoms worsened, and I had to wear a leg brace for over three years. I have had to use a cane for the last eighteen months. Pain was continuous, and the swelling of the knee was significant. I had difficulty sleeping, and started considering a total knee replacement procedure.
“A business associate mentioned that some friends had found relief from their osteoarthritis by using a home remedy. The remedy: each morning take two teaspoons, by mouth, of liquid pectin in four to six ounces of grape juice. The brand I use is by KRAFT FOODS, and carries the trade name Certo. It is commonly used to make fruit jams and jellies at home.
“My results: within eight (8) hours my pain and soreness diminished to almost zero; swelling was reduced significantly; and I slept all night without interruption for the first time in years; I stopped using the leg brace and cane that first day. These positive results have continued every single day since starting the regimen.
“I have no idea if I am one of a very lucky select few that can benefit from this remedy, or if it would have the same effect on most osteoarthritis-affected persons. I wish it could be the subject of a controlled study.
“My right knee is still arthritic bone on arthritic bone, but I have surprising mobility, and only very moderate discomfort.
“I am a very lucky guy! Thank you,” Kent
How to Mix Certo and Grape Juice:
Here is a video we created to show you how to make the Certo and Grape juice mixture. As an added bonus you will see how to whip up Sam Houston’s drink containing five parts grape juice, three parts apple juice, and one part cider vinegar. A daily dose of this potion (half a cup will do) is supposed to help relieve the aches and pains of arthritis.
Our readers often come up with intriguing work-arounds. This one comes from Gisella. ‘
It offers a somewhat complicated alternative to Certo:
“I have arthritis in my left thumb. This spring I got a steroid injection but while the injection was very painful it really did not give much relief.
“A friend of mine had told me about pectin, and I have been taking Ball powdered pectin for low sugar jams: 2 tsp in fresh apple cider that is available at stores in the fall. I actually first ferment the apple cider slightly with water kefir grains, and when I add the pectin it sort of reacts the way they advertise for Alka Seltzer.
“I finally have no pain in my left thumb which, at one point, was so bad I could not even drive. Once fresh apple cider is no longer available I will try the grape juice and am pretty sure that should work just as nicely. I also make our own milk kefir.”
Knox Gelatin
Brittle Nails
Report from reader:
“I had weak fingernails that split easily for years. Then I started taking one package of Knox plain gelatin daily. I usually mix it into my oatmeal.
“When I faithfully ingest an envelope of gelatin daily, I have extremely strong nails that never chip. If I stop, my nails begin to split again.
“Within two or three weeks of resuming the gelatin, my nails are once again almost indestructible. This remedy also works for my husband.”
Brittle nails are annoying but they do not cause the pain and disability of osteoarthritis. That’s why we were so interested to read reports from readers that gelatin can be helpful for sore joints.
We especially love to read dog stories:
“Gelatin worked well for me and my aging best-buddy canine. We both had joint problems and were beginning to limp slightly. I make a variety of Knox Gelatine-natural fruit smoothies for myself and mix it plain into my dog’s food daily. It has been a couple of months since I began using it and both my buddy and I have had remarkable success with the gelatin.”
More Readers report on Gelatin for Arthritis:
Q. I had been suffering with aching joints for a little over 10 years. Doctors didn’t pay attention because I’m only 37. Yet I could not move well and was in constant pain.
My mom read about taking gelatin to ease joint pain. I didn’t listen, but then she asked me to do her the favor of printing out some info on this subject off the Internet for a friend.
She’s very wise: the friend was me! She knew I would at least try it if I found others online with similar afflictions.
So I gave unflavored gelatin a try, a little bit in a glass of water. I was skeptical but by the third night, I was able to move my toes with no pain!
It had been a decade since I’d felt this good. In about a week and a half after starting, my hands were not swollen and I was able to type, brush my hair and do other tasks I hadn’t been able to do before. To me, it is a personal miracle.
A. We heard about this remedy for joint pain a couple of years ago from a reader who stirs a packet of Knox Gelatine into juice, oatmeal, soup or yogurt every day. You can read more about the history of Knox Gelatine on our website and read other stories from readers at this link.
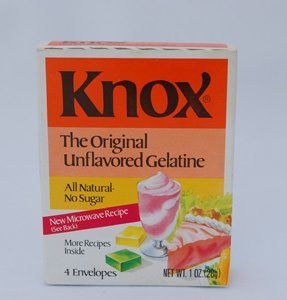
Knox Gelatin
When most people consider gelatin as a home remedy they think of strengthening brittle nails. We have been hearing about this approach for decades. The woman who wrote to us recently (see the story on the left sidebar) is just the last in a long string of readers who report success. Scientific support is thin. The best study we could find on gelatin was published in the AMA Archives of Dermatology (Sept. 1957). The researchers reported that:
“Forty-three of fifty patients with brittle nails who ingested gelatin daily for three months showed improvement in their nail structure.”
Gelatin for Arthritis:
We first heard about using gelatin for arthritis from Jonny L. He reported that:
“I’m writing to tell you about my excellent experience using gelatin for hip pain. I’ve had a chronic ache in my hip for several years. I’ve seen a chiropractor, whose ministrations were effective but temporary. Pilates helped for just a little while, and yoga had no effect. My doc took an X-ray and said she didn’t see any arthritis. The chiropractor said he did and told me to eat Jell-O.
“I decided to give it a try on the theory that it was perfectly harmless even if it didn’t work. For about six weeks I ate roughly half a packet of Knox Gelatine a day (prepared, not dry). No effect. But in a fit of hunger and frustration one day I gobbled up the remaining half pan, about two packets worth. The next morning I awoke completely pain free.
“I went online and found that people who use it recommend one packet a day. I’ve been doing that now for about two months, with only a very occasional twinge in my hip after driving for 12 hours. I don’t know why it started working, but since my hip doesn’t hurt, and it’s easy and cheap, I’m just doing it.”
This home remedy fits our favorite criteria: won’t hurt, might help and doesn’t cost too much. But is there any science to support it? Gelatin is made from collagen (the protein in connective tissue). It is tasteless and is used in food, pharmaceuticals (most capsules are made of gelatin) and cosmetics. Gummy candies are made from gelatin. So are marshmallows.
A double-blind, placebo-controlled, randomized, clinical trial using hydrolyzed collagen (fancy gelatin) to treat patients with osteoarthritis was published in the Journal of the Science of Food and Agriculture (March, 2015). The authors note that hydrolyzed gelatin is absorbed orally and “distributed to joint tissues and has analgesic and anti-inflammatory properties…Animal experiments have suggested that oral ingestion of collagen peptide might have beneficial effects on joint health such as OA [osteoarthritis].” In their human study subjects with knee osteoarthritis consumed collagen peptides in pill form.
The researchers concluded that collagen peptides are:
“effective supplements for the improvement in overall physical problems associated with OA and thereby help to improve the quality of life. It is hypothesised that the supplementation of collagen peptide regulates chondrocyte differentiation and stimulates synthesis of proteoglycans, resulting in the initiation of repair processes in cartilage tissue.”
In other words, there is scientific support for the idea that gelatin, which is hydrolyzed collagen, helps repair joint tissue and ease pain and inflammation. Once again, researchers have confirmed what our readers have been reporting to us for years.
Cherries and Gelatin:
Sometimes readers combine remedies. We found this story quite compelling:
“I am 55 years old and suffer from arthritis in my knees. One day I decided to try some unflavored gelatin with tart cherry juice because my nails were not growing as well as they used to, and gelatin is said to help with that. Tart cherry juice is supposed to be a good anti-inflammatory.
“Much to my surprise, the pain in my knees subsided substantially within a week! I had tried OTC pain relievers before to no avail.
“I now swear by this gelatin mixture I drink every morning. I find that if I miss my morning concoction, I feel pain before that day ends. Drinking it helps me so much that I go to the gym more often and have much relief from both the gelatin and the exercise. (My nails are no better, though.)”
Vinegar and Juice

A Reader Shares His Secret Vinegar Remedy:
Bud from Dallas shared this recipe with us many years ago:
“The man that once owned the Dallas Cowboys gave me his arthritis remedy and it’s been a godsend. It’s 1 teaspoon of a mixture of 50% apple cider vinegar and 50% honey (I mix a quart for a month or so supply) added to a 6-ounce glass of water with a teaspoon of Knox orange-flavored gelatin powder stirred in and dissolved. Within a few weeks I regained virtually 100% use of my knuckles which had really become stiff, sore, and painful to use! Exact measure of the three does not seem to be critical. I just eyeball them, stir, and drink. Hope it works as well for others as it does for me.”
The use of vinegar as a remedy dates back almost 4,000 years to the Babylonians, who reportedly used it to preserve food. Folklore has it that the father of modern medicine, Hippocrates, recommended vinegar and honey for a range of ailments over 2,000 years ago.
In the mid 20th century, D.C. Jarvis, MD, popularized the use of vinegar and honey in his book, Folk Medicine: A Vermont Doctor’s Guide to Good Health. He recommended a daily drink of eight ounces of water with two teaspoons of apple cider vinegar and two teaspoons of honey mixed into it.
It was supposed to help ease arthritis pain and prevent common health problems. Dr. Jarvis didn’t have the benefits of modern research on vinegar, so he had to use observational skills and his patients’ testimonies in building his arguments for honey and vinegar as a remedy.
As far as we can tell researchers have not invested resources to study Dr. Jarvis’ home remedy for arthritis. They have discovered that taking vinegar with a meal or just before it improves blood flow to the muscles and increases glucose uptake into muscle cells (European Journal of Clinical Nutrition, June, 2015; Journal of Diabetes Research, online, May 6, 2015.
As a result, blood sugar, insulin and triglycerides do not rise as quickly or as high after a meal as they would otherwise. The effect is most noticeable after a meal that has a lot of easily digested carbohydrates (European Journal of Clinical Nutrition, July, 2010). There is also some evidence that vinegar helps improve blood lipids and reduces inflammatory compounds in overweight teenage girls (Journal of Exercise Nutrition & Biochemistry, March, 2015).
Vinegar and Juice Recipes:
Over the years we have collected several vinegar and juice remedies for arthritis. Here are our favorites. We wish we had some science to support this approach. Sadly, this purely anecdotal.
Vinegar and Juice # 1
- 1 cup vinegar
- 1/3 cup honey
- 16 ounces grape juice
- 32 ounces apple juice
Drink a couple of ounces daily
Vinegar and Juice # 2
- 1 part cider vinegar
- 3 parts apple juice
- 5 parts grape juice
Drink 1/2 cup daily
Vinegar and Juice # 3
- 1 teaspoon orange gelatin powder
- 1/2 teaspoon apple cider vinegar
- 1/2 teaspoon honey
- 6 ounces of water
Stir ingredients together and drink daily
Pineapple (Bromelain)

A Story from a Reader:
“Several years ago friends told me that drinking a glass of pineapple juice every day helped them. I have found it to be more effective than the aspirin, prescription pain killers and acupuncture I had tried previously. It’s inexpensive, nutritious and has no side effects.”
Pineapple contains an anti-inflammatory enzyme called bromelain, and we have heard from a number of readers who swear by it:
Q. For several weeks, I’ve been experiencing moderate thigh and butt pain from osteoarthritis in my back.
I’m getting some moderate relief from meloxicam, an NSAID. But recently I am enjoying additional relief from eating fresh pineapple.
Not only is the pain greatly reduced, I’m able to walk with increased ease, stamina, and flexibility. What’s more, the pineapple is delicious.
I remember being given “ananase,” a pineapple derivative, to reduce swelling from an injury to my face decades ago. I assume that the active ingredient in my improvement is ananase, but I can’t seem to find this drug. Do you have any information on ananase?
Pineapple Compound
A. Ananase is also known as bromelain. In the US, bromelain is sold as a dietary supplement. This pineapple compound has been shown to reduce pain and swelling after molar extraction as effectively as the NSAID diclofenac (Journal of Oral and Maxillofacial Surgery, Jun., 2014).
Non-Drug Alternatives for Arthritis (Herbs & Spices)
Before aspirin, corticosteroids or nonsteroidal anti-inflammatory drugs, there were herbs and spices. During the eighth century, St. Benedict Crispus of Milan recommended cloves, pepper and cinnamon for the pain of an arthritic hip. In those days there were no double-blind, placebo-controlled scientific experiments to determine efficacy. People experimented with a wide variety of spices. During medieval times, spices were considered powerful medicines.
People in India have been using the bright yellow spice turmeric (Curcuma longa) for thousands of years. It was prized not only for its distinctive taste but also for its healing properties. Practitioners of Ayurvedic medicine were prescribing turmeric, frankincense (Boswellia serrata), ginger (Zingiber officinale) and Ashwagandha (Withania somnifera) for arthritis many centuries before western physicians learned about the anti-inflammatory properties of willow bark and aspirin.
Texas researchers note that Ayurveda:
“can serve as a ‘goldmine’ for novel anti-inflammatory agents used for centuries to treat chronic diseases.”
These hard-core scientists report that “Almost 200 Ayurvedic plants have been identified that exhibit anti-inflammatory activities” (Current Drug Targets, Oct. 1, 2011). In the pages that follow we will share some of our favorite herbs and spices to ease the inflammation of osteoarthritis.
Ashwagandha
Report from a Reader:
Elizabeth wrote to say:
“I have fairly severe osteoarthritis in my knees. I cannot take ibuprofen as I have had lapband surgery. Acetaminophen (Tylenol) is ineffective for the pain. The arthritis is quite debilitating and painful, and over time my flexibility and mobility have drastically declined.
“In the past I have tried various remedies including Glucosamine, Chondroitin, and turmeric. I think turmeric may help a bit, so I still take that. Recently I read of a study showing that Ashwagandha might help. I did some research and ordered one of the brands tested and approved by ConsumerLab.com.
“On the second day taking the Ashwagandha once a day (500 mg Withania somnifera extract (root) standardized to contain 2.5% withanolides), I awakened to find the pain had decreased dramatically. I’ve been taking it now for a week, and the pain is almost completely gone, however there is still some stiffness.
“I’ve never had anything make such a difference, and so fast, almost like someone flipped a switch. This is the first thing that has given me relief and I want to continue it, but would like to be sure it isn’t going to do any damage. Do you have any information you can share?”
Most people have heard of ginger and turmeric. Ashwagandha is a mystery to most westerners. It is officially Withania somnifera, and unofficially, Indian ginseng. Ingredients in the roots and leaves of this plant reduce inflammation through a variety of intriguing pathways. NF-kappa B activation is suppressed as well as TNF-alpha and COX-2. These are key targets for many pharmaceutical researchers.
Search PubMed, the U.S. National Library of Medicine, and you will discover hundreds of references on Ashwagandha. It has been studied for its ability to ease anxiety, calm an overactive mind and facilitate sleep. There is a suggestion that this plant has neuroprotective properties, meaning that it might be beneficial against Alzheimer’s disease and other dementias as well as enhance memory (Medical Hypotheses, July, 2016; Neurochemistry International, May, 2016; Biological and Pharmaceutical Bulletin, Vol 37, No. 6, 2014). The active ingredients, withanolides, may also have immune modulating effects and anticancer activity against a wide range of tumors (Toxins, May, 2016; International Journal of Molecular Sciences, March, 2016).
Arthritis:
As intriguing as Ashwagandha may be for a variety of other conditions, our primary interest in this plant is for its anti-inflammatory activity. A randomized, double-blind, controlled trial of Ashwagandha (brand name Sensoril) for knee osteoarthritis reported that one 250 mg capsule of Sensoril taken twice daily after meals produced “significant reduction in pain, stiffness and disability.” The authors noted that Ashwagandha has analgesic, anti-inflammatory, anti-arthritic and chondroprotective effects (Journal of Ayurveda and Integrative Medicine, July-Sept., 2016). The last means that it should be beneficial for joint tissue. Side effects included nausea and digestive upset, but no one dropped out of the study because of this adverse reaction.
We wish there were more human research on this natural product. The study described above was small. Animal research has been promising, but better clinical trials will be necessary before western physicians consider this fascinating plant an effective arthritis treatment.
The people at ConsumerLab.com tested a variety of Ashwagandha products and found that several did not pass muster. Pure Encapsulations Ashwagandha and Solaray Ashwagandha did meet their standards. As far as we can tell, ConsumerLab.com did not test the brand name product studied in the clinical trial described above. It is possible to purchase Sensoril Ashwagandha online from Amazon.
Cautions:
Side effects of Ashwagandha are primarily related to the digestive tract. Nausea, vomiting and diarrhea have been reported. Because this plant has anti-anxiety activity and is sometimes used to promote sleep, we recommend caution when it comes to driving or engaging in any activity that requires motor skills. Do not add Ashwagandha to other sedating medications.
The plant can also lower blood pressure and blood sugar, so do not combine it with medications for hypertension or diabetes unless a health professional with knowledge of its pharmacology is on board with the program. There is also some concern that it might increase thyroid hormone levels (Journal of Ayurveda and Integrative Medicine, Oct.-Dec., 2014). This may mean that Ashwagandha might be helpful for patients with sub-clinical hypothyroidism, but much more research will be required to demonstrate that. Our concern is that if it were added to standard thyroid treatment Ashwagandha might lead to thyroid overdose.
Boswellia
Reader Stories
Margot reports:
I’ve taken boswellia for years for both osteoarthritis and colitis. It cleared up the latter in a week and I noticed that my morning hip pain was gone as well. Here’s my advice for people who develop stomach trouble with it: take the minimum dosage–I find I can take one capsule every few days or at times weeks–and take it with a full meal.
Although many readers say boswellia does not work as well as other remedies, some do get good relief.
Such was the case with M.S.C.
“Boswellia seems to be practically a miracle drug for my arthritis pain. Have been able to cut way back (from 2/day to 1 or 2 per week) on Celebrex.”
Ayurvedic healers have also been prescribing boswellia (Indian frankincense) for arthritis. The name frankincense may ring a bell. Like myrrh, it is featured in the Bible story about the three wise men visiting the infant Jesus. That refers to Boswellia sacra, which grows in Somalia and Saudi Arabia. Indian frankincense comes from a different species, Boswellia serrata, a tree native to hilly regions of India.
In Ayurvedic medicine, healers have used boswellia to treat asthma, dysentery and skin disorders. Extracts have demonstrated anti-inflammatory activity. The independent and highly regarded Cochrane Collaboration analyzed the available scientific evidence on boswellia for treating osteoarthritis (Cochrane Database of Systematic Reviews, online, May 22, 2014).
Here were the conclusions:
“Five studies of three different extracts from Boswellia serrata were included. High-quality evidence from two studies (85 participants) indicated that 90 days treatment with 100 mg of enriched Boswellia serrata extract improved symptoms compared to placebo…The studies reported no serious adverse events.”
A small three-month trial carried out in Italy with a boswellia extract (FlexiCule) was effective in reducing pain, stiffness and improving walking distance without pain (Minerva Gastroenterologica e Dietologica, online, Oct. 22, 2015). We would be the first to acknowledge that large-scale, high-quality clinical trials involving boswellia are lacking.
Boswellia Side Effects:
This compound may cause reflux and symptoms of heartburn. Some people lose their appetite as a result. Readers have reported throat irritation and gastritis. One woman reported that her hot flashes “were back with a vengeance” after taking boswellia.
There is one case in the medical literature of a woman who ended up with a bezoar in her stomach. This is like a hair ball in a cat. Fiber and other material accumulate within the stomach or small intestine. She also had celiac disease, so it is hard to determine how likely this complication might be for those without celiac disease.
Boswellia should not be used during pregnancy. It may also interact with some prescription drugs.
Purchasing a high-quality boswellia supplement could be challenging. The FDA does not monitor such products. ConsumerLab.com found that Vitacost 5-Loxin met its standards and was reasonably priced. Other brands that passed muster by this testing organization included Instaflex Advanced and Solgar No. 7.
Turmeric (Curcumin)

Stories from Readers:
Health professionals are not impressed with anecdotes. We understand that such case reports are not considered scientific. But for the individuals involved, the n of 1 that represents their situation is all that matters.
Gerry in Hughesville, MD, reports:
“After years of suffering with arthritis in hands, elbows, knees and fingers, I read about tumeric and curcumin. I have been taking this combination supplement for 3 years and I have been pain free for a long time.
“I have only one side effect: The tips of my nails have turned a pale yellow from the turmeric. My doctor said “’stop worrying about all of these little things, and just cover your nails with nail polish.’ Halleluijah! It feels good to be pain free.”
Irene in McAllen, TX, shared this:
“I started taking turmeric for joint pain about three weeks after spending five days in the hospital for a necrotic antral stomach ulcer. It was caused by my use of ibuprofen and aspirin. I was told that I should try Tylenol and not take any anti-inflammatories anymore. I take Tylenol, which supposedly dulls the pain a little. (Not much.)
“I am drinking two cups a day of chicken bouillon in warm water with a level teaspoon of turmeric powder with a dash of black pepper; one cup in the midmorning and the second at dinner time. I think it tastes pretty good.
“The pain in my joints is much less and I plan to keep taking it. Turmeric powder is not expensive nor is instant chicken consomme. I am surprised at how well it has worked.”
Cindy in Ohio offers this interesting perspective:
“I just started taking one 800 mg capsule in the morning and another at night. It’s been a week now and the soreness in both my knees has improved greatly.
“I work with a few people who are from the country Nepal and they swear by turmeric. They told me to keep taking the capsules because they know I can’t use it in my food like they do. I don’t like the taste of it AT ALL.”
A newspaper column reader:
“For some time I have had increasingly bad pain in my right knee, left hip and lower back. I was getting so depressed because I was barely functioning.
“A friend recommended turmeric. Up to that point I had been living on way too much ibuprofen every day. Since the first turmeric tablet, I have not needed another ibuprofen. The results with turmeric are much better than with ibuprofen.”
Margaret in Ireland:
I’ve taken half a teaspoon of turmeric with some freshly ground pepper (to aid absorption) every day for a couple of months. The results are astonishing. My chiropractor is shocked. No more back pain, inflammation gone. It’s the best thing ever. Far better than painkillers.
Turmeric (Curcuma longa) has been revered in India for thousands of years. You know it as the ingredient in yellow mustard that will stain your clothes if you are careless and drip. Turmeric gives curry its wonderful color and flavor. Healers in China and India have been using turmeric for millennia. Long before molecular biologists started unlocking its anti-inflammatory secrets, people were using this amazing spice to treat a wide range of common conditions including digestive distress and arthritis.
Go to the U.S. National Library of Medicine (PubMed) and put turmeric into the search box. At the time of this writing you will find nearly 4,000 entries. Put curcumin, the active ingredient in turmeric, into your search and you will discover almost 10,000 articles, with more being added almost every day. That should give you some idea of the intense scientific interest in this ancient “golden” spice. Investigators are investigating curcumin for its potential benefits against cancer, cardiovascular disease, Alzheimer disease, ulcerative colitis and diabetes. For the purposes of this discussion, though, we are focusing on turmeric and curcumin against arthritis.
Anti-Inflammatory Activity:
Remember that healers in India figured out that turmeric had benefits against inflammatory conditions like arthritis centuries before researchers began unlocking the molecular mechanisms behind this activity. Scientists from Thailand offered the following (Journal of the Medical Association of Thailand, Jan. 2012):
“Nonsteroidal anti-inflammatory Drugs (NSAIDs) is one of the most commonly use medication for treatment of knee osteoarthritis which has the analgesic and anti-inflammation by inhibition of prostaglandin synthesis via COX-1 and COX-2 isoenzyme. The problem of prolong using NSAIDs has side effect on kidney, liver and GI system. Curcumin longa extract (Curcumin) is the Asian herbal medicine that has the anti-inflammatory effect by down regulate activation of NF-kappaB and proinflammatory cytokines such as Tumor Necrotic Factor-alpha, Interleukin-1, Interleukin-8, and Nitric Oxide Syntase.”
These authors are clearly not native English speakers, but they have described some of the anti-inflammatory mechanisms associated with curcumin. The systems they describe (tumor necrosis factor, NF-kappaB, etc.) are key signaling pathways for inflammation. A research paper in the highly regarded journal PLoS One (Dec. 30, 2015) notes that “curcumin is known to be effective in ameliorating joint inflammation in RA [rheumatoid arthritis}.” The investigators go on to describe the molecular mechanisms whereby curcumin restores healthier joint function. Curcumin alters dozens of factors that affect gene expression. This led a biologist at Texas Southern University in Houston to conclude (Biofactors, Jan-Feb., 2013):
“Based on its ability to affect multiple targets, curcumin has the potential for the prevention and treatment of various diseases including cancers, arthritis, allergies, atherosclerosis, aging, neurodegenerative disease, hepatic disorders, obesity, diabetes, psoriasis, and autoimmune diseases.”
Clinical Studies of Curcumin:
It is important to note that there is not a lot of incentive for researchers to perform randomized controlled trials (RCTs) of turmeric/curcumin. Because this spice has been available for thousands of years, no one can patent it. As a result, drug companies are not going to finance high-quality research. Government agencies tend to distrust dietary supplements, so resources are rarely adequate to conduct convincing research. That said, a meta-analysis of 12 RCTs concluded (Journal of Medicinal Food, Aug. 1, 2016):
“Although the exact biochemical cause of osteoarthritis remains unknown, it is associated with inflammation in articular cartilage, which can cause abnormal joint structure in the knee and hip and it is accompanied with pain. The most common treatments are analgesics and NSAIDs. However, the drugs have serious adverse events in the gastrointestinal tract and cardiovascular system. Therefore, herbal treatments that can mitigate the pain and inflammation have been investigated as potential primary or adjunct therapies for relieving arthritis symptoms. This systematic review and meta-analysis provided scientific evidence that 8–12 weeks of standardized turmeric extracts (typically 1000 mg/day of curcumin) treatment can reduce arthritis symptoms (mainly pain and inflammation-related symptoms) and result in similar improvements of the symptoms as ibuprofen and diclofenac sodium. Therefore, turmeric extracts and curcumin can be cautiously recommended for alleviating the symptoms of arthritis, especially osteoarthritis.”
Shopping for a Curcumin Product:
We suggest you check ConsumerLab.com before you shop to look for a brand that actually delivers what is promised on the label. About a third of the products that were tested did not come up to quality standards.
One of the world’s foremost researchers on curcumin is Ajay Goel, PhD. He is director of the Center for Gastrointestinal Research and of the Center for Epigenetics, Cancer Prevention and Cancer Genomics at the Baylor Research Institute. His research on BCM-95 curcumin makes this a leading candidate. There are a number of products containing this supplement, which meets Dr. Goel’s standards for research. You can find them in health food stores or online at Amazon.
Another research team used a proprietary product called Longvida® to treat pain and inflammation induced by exercise in muscles rather than joints (BBA Clinical, online Feb. 18, 2016). The dose used was 400 mg/day.
Side Effects of Turmeric:
It is important to remember that turmeric or its active component curcumin are not appropriate for everyone. Some people react with a severe skin rash signaling an allergy. Others find that such supplements cause digestive distress and don’t tolerate them for that reason.
Anyone who is taking warfarin (Coumadin) must not use turmeric or curcumin, as these products could increase the anti-clotting effect. It is possible that this interaction might also affect other anticoagulants, such as clopidogrel (Plavix) or even aspirin.
Turmeric might also lower blood sugar. People taking oral anti-diabetes medicines should monitor their blood sugar closely in case it drops too low as a result of this interaction.
People who are susceptible to kidney stones might wish to consider another approach to easing joint inflammation besides turmeric. It is high in soluble oxalate, which might increase the possibility of kidney stone formation (American Journal of Clinical Nutrition, May, 2008).
Ginger

Stories from Readers
P.C.M combines ginger & a dash of turmeric:
“I drink a cup of ginger tea with a dash of turmeric during a Rheumatoid Arthritis flare. The effect for me is similar to a dose of Ibuprofen: about 20 minutes after drinking the tea, I get considerable relief from both pain and swelling, and it lasts from four to six hours.
“To make the tea, I simply peel and slice a half-inch of ginger root into a cup of boiling water, cover, and steep for five minutes. Strain, add turmeric (only a dash, as it tastes quite strong), and sweeten to taste.”
C.P. likes ginger tea:
“I have been using ginger root in a large cup of green tea every morning (about one teaspoon) since October 2013. It has really worked for my osteoarthritis, especially in the knees.”
The history of ginger (Zingiber officinale) also dates back thousands of years to China and Southeast Asia. Chinese and Ayurvedic healers in India used this spice to ease nausea, vomiting, gas and stomach pain. Chinese sailors relied on ginger to control motion sickness. It was also used to relieve the inflammation and pain of arthritis.
Although our forefathers had no idea how ginger might be working to calm inflammation, research now shows that, like other herbs and spices, it can inhibit a variety of inflammatory promoters, including tumor necrosis factor-alpha and lipo-oxygenase. A review of randomized controlled trials published in the journal Osteoarthritis and Cartilage (Jan., 2015) concluded:
“Based on the empirical evidence, our data supports that oral ginger is able to reduce pain and disability in OA [osteoarthritis]…
“Since OA is a chronic disease with increasing need of treatment, it is important to find a right balance between benefit and harm with long term use of any applied treatment. NSAIDs are commonly used in OA, but serious cardio-vascular and gastro-intestinal adverse effects of this group of drugs are well-known. Ginger is, on the other hand, generally considered safe, and no serious adverse effects were seen when ginger extract was given to rats…Ginger therefore seems a better treatment option than NSAIDs judged on possible adverse effects of the latter treatment…
“The present meta-analysis on ginger for OA demonstrated that ginger has a superior effect on OA pain and disability to placebo, and apparently without serious adverse events. As a conclusion, ginger may be considered as part of the treatment of OA, where the patient is motivated for trying this nutraceutical.”
A Danish company, Eurovita, makes a purified ginger extract that has been studied in a clinical trial (Arthritis and Rheumatism, Nov. 2001). It is sold under the name Zinaxin. In this randomized clinical trial of Zinaxin the U.S. investigators concluded:
“A highly purified and standardized ginger extract had a statistically significant effect on reducing symptoms of OA of the knee. This effect was moderate. There was a good safety profile, with mostly mild GI adverse events in the ginger extract group.”
Side Effects of Ginger:
Although ginger is generally well tolerated, some people report stomach upset associated with supplements. Side effects may include belching, nausea and indigestion. There is also concern that ginger could interact with anticoagulant medications. That’s because it has some blood-thinning properties. Combined with drugs like warfarin (Coumadin), clopidogrel (Plavix) or ticlopidine (Ticlid), ginger might increase the risk of bleeding. Always check with a health professional who is knowledgeable about drug-herb interactions before adding a dietary supplement like ginger to an existing regimen.
German authorities recommend that pregnant women avoid ginger. Ginger is said to increase bile acid secretion. This is the reason people with gallstones or gallbladder disease are advised to avoid the herb unless supervised by a doctor.
Pycnogenol®

Nutritional supplement purple pills with empty blisters isolated on bold yellow background with copy space. Template for feminine beauty blog social media. Female healthcare concept
One dietary supplement for arthritis pain that might not be on your radar is Pycnogenol®. This is a polyphenol-rich extract from the bark of the French maritime pine. In a month-long study, one group of people with finger pain due to arthritis took Pycnogenol in addition to standard care, while a second group got standard care only (Minerva Surgery, Oct. 2024). By the end of the study, those on the supplement had improved their grip strength and reduced their inflammation. In comparison to those using oral diclofenac showed greater pain relief for those taking the pine bark extract.
The hands and fingers are not the only joints that seem to benefit. A review of three randomized placebo-controlled trials found that Pycnogenol reduced joint stiffness remarkably as well as reducing joint pain (Journal of Medicinal Food, Jan. 2018). Although all volunteers in these trials were allowed to use NSAIDs as needed for pain relief, those taking Pycnogenol ended up taking much less NSAID medication than those in the placebo groups. No serious safety problems were detected.
Another review found that Pycnogenol, like Boswellia and turmeric, seemed to offer significant pain relief in the short term (British Journal of Sports Medicine, Feb. 2018). Very few of the studies have evaluated long-term effects, either positive or negative.
How Does It Work?
One study identified a possible mechanism. The investigators administered Pycnogenol or nothing to patients scheduled for knee replacement surgery (BMC Complementary and Alternative Medicine, Dec. 16, 2017). The knee cartilage removed during the surgery demonstrated down-regulation of cartilage-degrading genes in the people who had taken Pycnogenol compared to those who had not. Cellular markers of inflammation were reduced.
The most recent study compared ultrasound images of the affected joints along with laboratory measurements of inflammation markers such as CRP (Minerva Surgery, Feb. 2024). In addition to 20 patients who got standard arthritis treatment, 25 took two supplements: 150 mg Pycnogenol® and 450 mg Centellicum daily. The ultrasound images revealed an advantage to the supplement group after six months. They also had better fitness and function, lower pain scores and reduced levels of C-reactive protein, a measure of inflammation.
None of these studies would really be considered quite gold-standard, even though they were controlled trials. Moreover, many of them were supported by the maker of Pycnogenol, Horphag Research. Consequently, it would be wise to consider these rather glowing results with some caution. The benefits and apparent tolerability of the supplement might well make it worth a try, though.
Stinging Nettle
Another natural remedy for arthritis is stinging nettle (Urtica dioica). An extract or tea made of leaves and stems can be taken for joint pain. According to herb expert James Duke, PhD, some people with access to fresh leaves “sting” themselves on the sore joints to achieve symptomatic relief.
That seemed a bit masochistic to us, but to our surprise we found that British physicians had actually tested this approach for thumb and finger arthritis. A controlled trial of such “nettle sting” therapy published in the Journal of the Royal Society of Medicine (June, 2000) confirmed that it produced a statistically significant improvement over the placebo deadnettle leaf (Lamium album).
Not surprisingly, research has demonstrated a variety of anti-inflammatory mechanisms associated with stinging nettle (Seminars in Arthritis and Rheumatism, June, 2005). Authors of this study note that stinging nettle capsules may cause upset stomach and rash and they warn that “Caution should be used when used with sedatives, diabetic medications, and antihypertensive medications.”
Apitherapy (Bee Stings) for Arthritis

Stories from Readers
“I’m a nurse in a rural hospital. Some of the mountain folk I care for tell me that a bee sting every two years or so will significantly decrease arthritis inflamation and pain. They attribute this remedy to the Chinese who came to this area to work on the railroads and logging industry.”
G. Gordon shared his heritage:
“My dad was a bee farmer from age 17 to 82. All of his siblings suffered from bad arthritis. When dad died at age 82 his hands looked better than mine do at at 43.
“Getting stung was a regular part of our childhood since we had over 200 hives on the property at all times. I also remember people coming to the farm for stings. They’d sit on the rock benches and dad would catch bees and sting them.”
Ann T remembers her childhood:
“When I was about 10 years old, I had severe pain in both knees. Doctors believed it to be arthritis (even in such a young child) and treated me with painkillers–without success. My parents, who were from Ukraine, took me to a beekeeper friend. Over two summers I was stung behind the knees several times during the course of each summer. The arthritis type pains were gone for many years and only started to come back in my mid-forties. I’m seriously thinking of doing this again.”
Frank in Gulfport, MS, had a nasty surprise:
“I was recently stung multiple times by yellow jackets on my legs, buttocks, arms and chest. I estimate upwards of 30 times. The pain was excruciating and lasted approximately 20 hours.
“I have a knee replacement in one knee and osteoarthritis in the other. After the pain from stings subsided I noticed a dramatic relief of pain in my knee joints. At first I thought I was imagining the change. But as the days went by I had to accept the relief was real. I’m able to rise from a sitting position without using my arms for support and am able to walk with much less pain. Go figure. (I am over 90 years of age.)
Of course, we would discourage anyone from repeating such an accidental “experiment.” That many yellow jacket stings could be life threatening!
Speaking of stings, most of us try hard to avoid being stung by a bee. There are others, however, who actually seek out people who are skilled in the ancient art of apitherapy.
It comes as a surprise to health professionals to learn that apitherapy has a history that stretches back thousands of years. Practitioners use bee pollen, honey, royal jelly and bee venom. For this discussion, we will focus on bee venom therapy or BVT. In a nutshell, it involves controlled honey bee stings in areas of inflammation.
Bodog F. Beck, MD, wrote a book in 1935 titled Bee Venom Therapy: Bee Venom, Its Nature, and Its Effect on Arthritic and Rheumatoid Conditions. Not surprisingly, it was panned in the pages of the Journal of the American Medical Association, (June 8, 1935) for being “uncritical” and folksy. But Dr. Beck treated a great many patients in New York City, where he practiced medicine for decades. There were even brand-name products such as Apiven, Imminim and Venapis that could be administered by injection. Practitioners who relied upon actual bee stings suspected that the “drugs” lost potency as a result of the purification process.
In some sense, BVT was immunotherapy, in that it may have modified or retrained the body’s immune reaction. The response to the stings appeared to calm inflammation for long periods of time. Some patients were reported to remain symptom-free years after a full course of treatment was completed.
There is some animal research to support the concept. Korean scientists tested bee venom (BV) in a rat model and concluded, “whole BV was found to inhibit arthritis inflammation and bone changes in the rat. This may be an alternative treatment for arthritis in humans” (In Vivo, Jul-Aug, 2005).
A randomized trial in China compared bee venom therapy with medications (methotrexate, meloxicam and sulfasalazine) for easing symptoms of rheumatoid arthritis. Patients who received the BVT had a better response on symptoms of joint swelling, pain, and morning stiffness than the medication group. The authors concluded:
“Combined application of bee-venom therapy and medication is superior to simple use of medication in relieving RA [rheumatoid arthritis], and when bee-sting therapy [is] used, the commonly-taken doses of western medicines may be reduced, and the relapse rate gets lower.”
We only wish there were large-scale clinical trials to test the immune modifying impact of BVT on arthritis, particularly osteoarthritis. There is substantial interest in both China and Korea, so perhaps these countries will do the heavy lifting required to demonstrate both the mechanism of action and the clinical reality of this approach.
Is BVT a Placebo Response?
When we mention bee venom therapy to health professionals, they frequently invoke the familiar refrain that it must be a placebo response. That is to say, it’s psychological–all in the person’s head, not a “real” physical reaction. We have received a number of stories from people who were totally unprepared for the results, like this person:
“While snoozing on the porch I was stung on the finger by a tiny bee. The result: intense pain, and after that a great reduction of arthritis in my arm.”
Some people report accidental benefit from other stings, such a yellow jackets or fire ants.
SweetDoug offered this yellow jacket story:
“I’ve had arthritis in my big right toe for years, starting in my early 40’s due to an injury I sustained in high school, where a bench fell on my toe.
“This summer, I had some yellow jackets in the house. They disappeared, but what happened was, they just dropped onto the floor. Well, guess who stepped on one. Eee-yowwwwwww! Yup. Right on the foot, under the middle toe.
“A day later, my big toe was not aching, and it’s not ached for several months. It’s just now coming back. I’m going to do this again next spring when the little buggers come out again.”
John in Florida shared this intriguing fire ant story:
“I am in my 30s and in declining health, I moved to Florida from a state that’s too cold for fire ants.
“I have chronic nerve pain that is never ending and that runs down both legs. I was out walking (it helps me to spasm less) and I got bit for the very first time by a fire ant on my big toe, and it hurt. But ten minutes later the pain and spasm in the leg I was bitten on stopped, but not in the the leg that wasn’t bitten.”
We have collected lots of interesting anecdotal reports (see the side bar for more stories from readers). We only wish modern medicine would study this ancient arthritis treatment in a scientific manner. We need large clinical trials to convince skeptics this is more than a placebo response. You can listen to a radio show we did on this topic at this link.
People with bee-sting allergies MUST avoid this remedy! Anyone who considers apitherapy will need to find an experienced practitioner who is prepared to treat a severe allergic reaction such as anaphylaxis. Stings from any animal can be extremely dangerous! Learn more from the American Apitherapy Society.
Acupuncture for Arthritis

Stories from Readers:
Jim in Seattle says:
“I just hurt my knee a few weeks ago and had acupuncture after limping around all week. The first treatment took the pain away. Then in two days it returned and I went back for another treatment. Pain is gone! It’s been a month and the pain has not returned.”
Ann in Durham, NC, says:
“My husband has been receiving acupuncture for knee pain for several months with relief from pain. We understand this relief is similar to taking a pain reliever (without the drugs). It doesn’t cure the underlying problem, but it gives relief so he can resume exercise to build up leg muscles.”
Acupuncture has been used in China for thousands of years. It involves the placement of extremely fine needles in special acupuncture points throughout the body. Western medicine generally disparages acupuncture and traditional Chinese medicine. That’s because the meridian system of energy flow cannot be seen or measured in the human body the way nerves and blood vessels are. Doctors can watch blood coursing through arteries and veins. The idea of life-energy or “qi” has no framework in standard medical education. If you can’t see or measure it, the thinking goes, how could it exist?
Not surprisingly, if you don’t believe something exists, you won’t study it. There have been relatively few scientific studies of acupuncture for arthritis in the west. Researchers in other countries do report some success. Orthopedic surgeons in Shanghai performed a meta-analysis of 14 randomized controlled trials involving 3,835 patients with knee osteoarthritis (Saudi Medical Journal, May, 2012). They concluded:
“Acupuncture provided significantly better relief from knee osteoarthritis pain and a larger improvement in function than sham acupuncture, standard care treatment, or waiting for further treatment.”
The Cochrane Database of Systematic Reviews (Jan. 20, 2010) concluded that “sham-controlled trials show statistically significant benefits” from acupuncture. But the authors go on to say the benefits are small and may be due in part to “expectation or placebo effects.” We agree with these experts that pain relief is probably modest.
A systematic review of nearly 18,000 patients suffering from chronic pain and osteoarthritis concluded that benefits often last well after the treatment ends (Pain, online, Oct. 17, 2016). Chinese physicians compared physical therapy with acupuncture in patients with knee osteoarthritis (American Journal of Translational Research, online, Sept. 15, 2016). They measured pain, stiffness, physical function and cartilage repair (using MRI scanning). Those patients randomized to receive acupuncture performed better on all measures than the people who only received physiotherapy. The authors concluded that “acupuncture is a feasible alternative therapy for KOA [knee osteoarthritis) patients.”
Sadly, acupuncture is rarely covered by insurance. As a result, many people won’t be able to afford several months of treatment. Others are squeamish about the thin needles even though most people find them quite tolerable. Acupuncture may be worth a try on the grounds that it might help and is unlikely to cause the serious complications associated with corticosteroids or NSAIDs. We would not predict miracles, however.
Other Options

Stories from Readers:
Perry in San Diego:
“I know glucosamine HCL works for me. I have degenerative joint disease affecting my spine and hands. I have been taking glucosamine HCL since it was first offered in the US.
“When I take it, my range of motion increases and my discomfort decreases. I’m sure it’s not placebo because there have been times I have forgotten to buy it and gone for a few weeks without it. My joints always remind me and when I start taking it again I get the same positive effects. I practiced chiropractic for 30 years and I prescribed it routinely for my patients. Most of them related it helped them. It is not a cure, but it does offer some relief and does not increase the risk of stroke like many NSAIDs do.”
Robert in Virginia:
“My wife and I are in our mid 60’s. We had taken glucosamine and chondroitin for many years and found it effective for reducing joint pain. However, after hand surgery for arthritis, my wife developed a nodule diagnosed as Dupuytren’s disease. She quit glucosamine & chondroitin and the growth was dramatically reduced.
“I quit the combination when I read that chondroitin was associated with the spread and recurrence of prostate cancer. Apparently, glucosamine may not be as big a problem. Yet the recommendation is that men should stay off chondroitin if they have prostate cancer or are at high risk of prostate cancer. As a substitute, I’ve found glucosamine and MSM [methyl sulfonyl methane] to be effective.”
William offers a short story:
“I can’t speak for osteoarthritis of the knee. My thumb was hit by a waterlogged softball as a teen and if I do not take glucosamine and chondroitin it hurts. If I do, it doesn’t.”
Side Effects of G&C?
Some people report elevated cholesterol levels. Others worry about blood sugar:
Lucy & Penelope reported:
“Glucosamine chondroitin pills caused my LDL cholesterol to go up 40-50 points! When I stopped G & C the numbers went right down again.”
“Lucy, that was my experience too. Be sure to check that it’s not sending your cholesterol through the roof!”
We have come to believe that osteoarthritis is not one single entity but rather a somewhat mysterious condition that affects different people differently. Some experience intense pain in a hip but not in fingers. Others complain about their knees and their fingers but not their hips. For some people there is minor disfigurement, such as bent or crooked fingers, but very little pain. Other individuals have pain that comes and goes unpredictably. We have heard from senior citizens who have “bone on bone” in their knees but are able to exercise with minimal pain. Others have normal-looking x-ray images or CT scans, but are in excruciating pain.
There is no one treatment that works for everyone. There are many people who get by beautifully with ibuprofen, naproxen or prescription celecoxib (Celebrex). These NSAIDs help them function and they experience few, if any, side effects. Other people experience a whole gamut of complications from hypertension and stomach ulcers to heart attacks or heart failure.
A home remedy that works for one person (Certo and purple grape juice) may be totally worthless for someone else. Hundreds swear by the benefits of gin-soaked raisins while many scoff that it’s pure placebo. We cannot predict what might work for any given individual. Neither can a rheumatologist. Much of this is trial and error. Here are several more options that may be worth consideration.
Glucosamine and Chondroitin
Ever since Jason Theodosakis, MD, wrote his giant bestseller, The Arthritis Cure, glucosamine and chondroitin (G&C) have been the most popular alternative treatments for osteoarthritis. The promise was that these dietary supplements would relieve pain and inflammation and repair damaged cartilage. How good is the evidence that G&C live up to this reputation?
Over the years there have been numerous studies published in medical journals. A review in JAMA (March 15, 2000) of all the studies published between 1966 and 1999 concluded:
“Trials of glucosamine and chondroitin preparations for OA [osteoarthritis] symptoms demonstrate moderate to large effects, but quality issues and likely publication bias suggest that these effects are exaggerated. Nevertheless, some degree of efficacy appears probable for these preparations.”
Another analysis of 15 well-conducted trials of G&C for knee arthritis concluded that there was “structural efficacy” but called for further research (Archives of Internal Medicine, July 14, 2003). So far, so good. People with arthritis had reason to believe that their investment in G&C products would pay off in terms of symptomatic relief and joint protection.
Then came the big disappointment. The National Institutes of Health funded the largest, most expensive ($14 million) and most definitive clinical trial ever undertaken to determine the effectiveness of G&C. Nearly 1,600 patients were recruited from 16 academic rheumatology centers around the United States. GAIT—Glucosamine/Chondroitin Arthritis Intervention Trial—was the Big Kahuna of clinical studies. These dietary supplements were going to be tested as if they were standard drugs. Subjects were randomly assigned to receive glucosamine, chondroitin, G&C together, Celebrex, or placebo. Investigators were looking for a relatively modest 20 percent improvement in knee pain by the end of 6 months.
The envelope was opened at the 2005 Annual Meeting of the American College of Rheumatology. Daniel Clegg, MD, chief of the Division of Rheumatology at the University of Utah School of Medicine, announced the findings:
“As expected, celecoxib [Celebrex] improved knee pain in patients with osteoarthritis. For the study as a whole, the supplements [glucosamine and chondroitin] were not shown to be effective.”
Wow! This multimillion-dollar, comprehensive trial had laid a giant goose egg. Here’s the straight and skinny on GAIT. Patients with mild knee pain saw no statistical improvement while taking G&C compared with placebo; 62.9 percent responded to glucosamine and chondroitin given together, whereas 61.7 percent got benefit from placebo and 70.3 percent responded to Celebrex.
The investigators did report that “an exploratory analysis suggested that the combination of glucosamine and chondroitin might be effective in osteoarthritis patients who had moderate to severe knee pain.” This subset of patients with worse pain did appear to get statistically significant benefit: 79.2 percent on G&C experienced pain relief compared to 69.4 percent on Celebrex and 54.3 percent on placebo. These results were not overwhelming, though, since the researchers were careful to qualify the data as “exploratory” and the result as “might be effective.” When the patients with “moderate to severe” osteoarthritis were lumped together with those with “mild” arthritis, there was no statistically significant improvement compared to placebo. All in all, we would have to say that the outcome of this gigantic U.S. study was disappointing.
European Study Shows Benefit
That said, there are a great many people who swear that glucosamine and chondroitin work wonders for them. A European study lends credence to their experience (Annals of Rheumatic Diseases, online, Jan. 14, 2015). In this randomized, controlled trial, glucosamine and chondroitin were compared to the prescription arthritis drug celecoxib. The study was conducted in four European countries and involved more than 600 subjects with painful knee osteoarthritis.
The clinical trial lasted for six months. At the end, both groups had only half as much knee pain as when they started. They also had less joint swelling and stiffness.
Why the Difference?
We have long wondered why veterinary and European research so frequently shows benefit from glucosamine and chondroitin, while the US trials nearly always reveal these supplements to be ineffective. The authors point out that the European versions of glucosamine and chondroitin are treated as prescription medications and carefully regulated. U.S. supplements may be less reliable.
A recent Spanish study found, however, that people with knee osteoarthritis did not fare better on a combination of glucosamine sulfate and chondroitin sulfate than on placebo for pain and function (Roman-Blas et al, Arthritis & Rheumatology, Jan. 2017). The authors suggest, however, that further research might help determine who could benefit from this nutraceutical.
Based on these results, glucosamine sulfate and chondroitin may provide anti-inflammatory pain relief for those who cannot tolerate non-steroidal anti-inflammatory drugs. Again, trial and error are the best way to determine whether this supplement will work for you.
MSM & SAMe
Stories from Readers
Patricia describes her “cocktail”:
“I have been taking 1/8 tsp of pure MSM for the arthritis in my knees for more than 2 years with outstanding results. MSM is mixed in a cocktail consisting of POM and grape juices and two tbsp of apple cider vinegar. I drink it while eating dinner.
“At the onset, I drank this cocktail twice a day for a month to enhance its effectiveness. The twice a day regimen is also used when rain is imminent. After it rains, I drink it once a day. After conferring with my doctor, I bought one online at a lower cost.
“At 67 years young, I am once again very active and enjoying the sport activities of my youth.”
Elaine in Florida wrote:
“I got no relief for lower back osteoarthritis with glucosamine & chondroitin. But a friend said her rheumatologist recommended glucosamine plus MSM, so I tried that and got great results.”
A Story from a Reader
LadyLiza shared this experience:
“Here is a list of supplements that have helped me immensely with my hip arthritis. I am no longer crippled with pain. I have no pain at all.
“I started with niacinamide at my doctor’s suggestion. I added 2200 mg of turmeric daily in divided doses and increased it up to around 4000mg/day. But since I don’t like the taste, even in the pills, I searched for something different.
“Then I tried SAMe, and that killed most of the pain. I started with 200 mg am and 200 evenings. Make sure you are taking a vitamin B complex at the same time so that all the effects of SAMe are apparent. Some of this info comes from my physician, who also has a PhD in nutrition.
“This was wonderful for me because it also helps with depression and when I get into a lot of pain, I get depressed. I am 65.”
Methylsulfonylmethane (MSM) is a naturally occurring compound found in many fruits and vegetables. It has been widely promoted as an arthritis remedy, but there is little clinical research to support the testimonials. A randomized controlled trial published in the journal Osteoarthritis and Cartilage (March, 2006) reported a statistically significant improvement in OA symptoms with MSM. The conclusions:
“MSM (3 g twice a day) improved symptoms of pain and physical function during the short intervention [12 weeks] without major adverse events. The benefits and safety of MSM in managing OA and long-term use cannot be confirmed from this pilot trial, but its potential clinical application is examined.”
Another double-blind, controlled clinical trial of MSM was published in BMC Complementary and Alternative Medicine (online, June 27, 2011). The authors were equally cautious with their conclusions:
“Patients with OA of the knee taking MSM for 12 weeks showed an improvement in pain and physical function. The results suggest that larger and long-term studies may find additional and greater improvements in knee OA symptoms. These improvements, however, are small and it is yet to be determined if they are of clinical significance.”
Despite the lack of scientific proof, some readers do report success with this dietary supplement. We heard from one postmenopausal woman who reported that MSM not only eased her arthritis pain, but also had some unexpected benefits:
“I went to my local natural pharmacy and said I was taking glucosamine and chondroitin because when I hit menopause I developed arthritis pain in my hands. The folks there suggested I take MSM as well. They said to increase the dose gradually because it gives you diarrhea if you bump it suddenly. I’m taking a great deal of it and I have no unpleasant side effects. It controls the pain beautifully.
I did discover one fantastic side effect. I was also having another issue with menopause. My hair was thinning, falling out in clumps. But as soon as I started taking all this MSM my hair became gorgeous, my skin soft, and my nails fantastic. I look beautiful! I’m going to be 55 soon and my husband says I look at least 10 years younger.”
This woman was not the first to report that MSM helped her hair. Sadly, though, we could find no scientific support for this claim.
SAMe (S-adenosylmethionine)
Here is what the Mayo Clinic has to say about this fascinating compound:
“SAMe is made in the body from a reaction between methionine, which is an essential amino acid, and adenosine triphosphate, a molecule that carries energy. SAMe is involved in many different reactions in the body.”
We wish there were more and better well-controlled clinical trials of SAMe. We rely on the independent Cochrane Collaboration to evaluate a variety of medications and natural products. In the case of SAMe, the experts for Cochrane concluded in 2009 that their:
“current systematic review is inconclusive, hampered by the inclusion of mainly small trials of questionable quality. The effects of SAMe on both pain and function may be potentially clinically relevant and, although effects are expected to be small, deserve further clinical evaluation in adequately sized randomised, parallel-group trials in patients with knee or hip osteoarthritis.”
In 2004 researchers at the University of California, Irvine, reported on a small double-blind cross-over study (BMC Musculoskeletal Disorders, Feb. 2004). Patients with osteoarthritis of the knees were given either 1200 mg of SAMe per day for eight weeks or 200 mg of celecoxib (Celebrex). Neither the investigators nor the subjects knew who got what. There was a one week washout period and the patients were crossed over to the other treatment. The study lasted for 16 weeks. Everyone was tested for pain control and functional improvement. It turned out that SAMe took a little longer to go to work. The effects were not instant, but only showed up after about a month. During the second month of treatment SAMe was equal to celecoxib in both pain relief and joint function. The investigators concluded:
“SAMe is helpful for the management of pain in osteoarthritis, and demonstrates similar effectiveness as a currently accepted COX-2 inhibitor celecoxib. Results from this study add and confirm results from prior studies indicating a possible role for SAMe in the management of osteoarthritis.”
Korean researchers also compared SAMe to an NSAID: nabumetone (Relafen). The scientists concluded (Clinical Therapeutics, Dec. 2009):
“This study found no significant differences in pain relief or tolerability between treatment with SAMe or nabumetone over 8 weeks in Korean patients with knee OA.”
It is nice to know that a natural product like SAMe works as well as NSAIDs. As far as we know, SAMe does not carry the cardiovascular risks or other side effects associated with NSAIDs. It would be nice if researchers took this dietary supplement a bit more seriously and conducted some longer well-controlled trials.
Avocado/Soybean Unsaponifiables
One of the popular nutraceuticals people take to manage arthritis pain is something called ASU–avocado/soybean unsaponifiables (Ragle & Sawitzke. Drugs & Aging, Sep. 2012). It is made from a third avocado oil and two-thirds soybean oil and contains compounds that don’t combine with alkalines to make soap. (Go figure!) This supplement appears to be safe, and may help people use less NSAID medication for joint pain. But as with many other dietary supplements, the results of studies on its efficacy have been inconsistent.
Scientists have found a number of inflammatory pathways affected by ASU. In the laboratory, this compound promotes collagen repair, and in the clinic it reduces pain and stiffness (Christiansen et al, Cartilage, Jan. 2015). The usual dose of ASU is 300 mg/day, and experts recommend a trial for three months to see if it will help. There are hints that people with osteoarthritis of the knee are more likely to benefit than those with osteoarthritis of the hip (Christiansen et al, Osteoarthritis and Cartilage, April 2008).
Hyaluronic Acid
Hyaluronic acid, also called hyaluronan, is a naturally occurring compound that is abundant in the synovial fluid in joints. It is also an important component of joint cartilage. It isn’t surprising, then, that rheumatologists have tried injecting hyaluronic acid into arthritic joints to see if they improve.
A review of research has found that injections of hyaluronic acid into the joints works at least as well as standard arthritis treatments, with a favorable safety profile (Cooper et al, Arthritis Care & Research, online Jan. 24, 2017). A multi-center study of about 100 patients found that combining injections of hyaluronic acid with platelet-rich plasma provided greater relief of knee pain due to osteoarthritis than either treatment alone (Lana et al, Journal of Stem Cells & Regenerative Medicine, Nov. 29, 2016).
An economic analysis based primarily on European data determined that the use of high-molecular weight hyaluronic acid injections is cost-effective for treating knee osteoarthritis (Hermans et al, Arthritis Care & Research, online March 20, 2017). Needless to say, an injection into the joints is not a do-it-yourself proposition. If you want to try this, you will need to find a physician who is enthusiastic about it.
Platelet-Rich Plasma
If you do find a doctor who is interested in such injections, you might discuss platelet-rich plasma (PRP). A recent meta-analysis of 12 clinical trials compared the outcomes of hyaluronic acid injections with injections of platelet-rich plasma (Hohmann et al, European Journal of Orthopaedic Surgery & Traumatology, online Feb. 14, 2020). The researchers found no differences in “clinical outcomes” after six months or a year, but they did find that people who got PRP injections of their own plasma reported significantly less pain. These studies focused on osteoarthritis of the knee.
In Conclusion
Osteoarthritis remains a mystery. Health professionals do not know exactly what causes it and certainly do not know how to cure it. When most patients visit a primary care physician or a rheumatologist and complain about stiff or painful joints, out comes a prescription for an NSAID. There just aren’t a lot of FDA-approved arrows in the quiver.
By now, you know the potential adverse effects of NSAIDs, especially when taken in high doses for long periods of time: hypertension, fluid retention, heart attacks, strokes, irregular heart rhythms (atrial fibrillation), congestive heart failure, indigestion, ulcers, perforation of the stomach and/or intestines, kidney damage, severe allergic reactions, liver damage, blood disorders and breathing difficulties (worsening asthma).
Most doctors have become reluctant to prescribe corticosteroids for osteoarthritis and with good reason. Just go back and review the complications of long-term prednisone therapy at the beginning of this discussion. Increased risk for diabetes, hypertension, osteoporosis, fractures, ulcers, cataracts and glaucoma are just a few of the side effects associated with corticosteroids.
What’s left? We have tried to provide you with a variety of non-drug options for controlling inflammation and pain. We hope we have not overwhelmed you with possibilities. Is there one best treatment? Absolutely not! As already mentioned, what works for one person may be absolutely worthless for someone else. As you have read, many people find home remedies like gin-soaked raisins or Certo and grape juice quite helpful. Others prefer gelatin or turmeric. What no one knows is whether a combination of things works better than one thing alone.
There may be synergy between some of these remedies. One person may find that combining acupuncture with curcumin and tart cherry juice is the magic formula. Another person might discover that applying Voltaren Gel to sore joints, taking the herb boswellia and drinking grape juice and Certo does the trick.
None of these approaches is a substitute for good medical management. Blending home remedies with medications such as salsalate may offer the maximum benefit. Below you will find an overview of our recommendations:
• Preventing arthritis beats trying to treat it. Keep weight under control, drink fresh-squeezed orange juice, and follow a Mediterranean diet. Get 10 to 15 minutes of sunshine on your face and hands several days a week or take around 2,000 IU of vitamin D daily.
• Aspirin is the best buy in the pharmacy. It relieves pain and inflammation while reducing the risk of heart attack, stroke, and many cancers. Beware of its potential to cause ulcers or interact with prescription drugs. Medical supervision is essential for long-term use.
• Topical NSAIDs reduce the risk of stomach irritation and ulceration. Pennsaid and other prescription NSAID creams and gels will require a doctor’s prescription. A compounding pharmacist in the United States can make a ketoprofen gel or cream without a prescription.
• Fish (or fish oil) can supply valuable omega-3 fatty acids. These anti-inflammatory compounds are helpful against heart disease, arthritis, and other chronic conditions.
• Home remedies such as gin-soaked raisins, Certo and grape juice, gelatin or vinegar and juice may be effective. Other juices that may have anti-inflammatory benefits include pomegranate, pineapple and cherry.
• Turmeric is a spice that does triple duty. It comes from the ancient Ayurvedic healing tradition and may relieve inflammation. In addition to joint pain, some people find that it helps psoriasis. It’s also being studied for its effects against a wide variety of cancers.
• Glucosamine and chondroitin remain controversial. People with moderate to severe pain may benefit from its use even though those with mild arthritis probably won’t.
• Acupuncture or apitherapy may offer significant pain relief. Seek a qualified acupuncturist or apitherapist for such treatment.
In summation, use common sense! If something isn’t working, consider moving on to something that does. If you experience side effects, whether from an OTC pain reliever or an herb, stop and consult a physician. Just because something is labeled natural does not mean it will be safe for you. Herbs and dietary supplements can produce adverse reactions in some people.
Publication Information
Published on: February 26, 2024
|
Last Updated: December 16, 2024
Publisher: The People's Pharmacy
© 2026 The People's Pharmacy
