
isOne of the more troubling complications of long COVID is something called postural orthostatic tachycardia syndrome, or POTS for short. This is a mysterious condition that is often diagnosed when everything else has been ruled out. A big symptom is lightheadedness upon standing. Some people faint! Other symptoms to be aware of are nausea, palpitations and rapid pulse, blurry vision, brain fog, fatigue, inability to exercise, head pain, and shaky hands. Is there a way to help POTS by stimulating the vagus nerve?
POTS and the Autonomic Nervous System:
Most people are familiar with the “sympathetic” nervous system. This has been crudely categorized as the “flight or fight” response to a threat. The idea is that when you see something scary approaching (the most common example is the now-extinct sabre-toothed tiger), our sympathetic nervous system goes into high gear.
The modern-day equivalent would be a flashing blue light in your rear view mirror. When you look down at your speedometer you discover that you were driving over the speed limit. The flashing blue light is from a police car! That tends to cause an adrenaline rush.
Adrenaline (aka epinephrine) starts to flood our system. Our heart beats faster and harder, our pupils dilate (to see things at a distance better) and our lungs dilate so we can breathe in more oxygen. All this allows us to run away or stand and fight. Of course that would not be such a good idea if we were in fact speeding.
The “parasympathetic” nervous system is the so-called “rest and digest” system. When activated, our pulse slows, our heart beats less forcefully and our pupils constrict so we can see things closer rather than farther away. We make more saliva and our digestive tracts go back to work when our vagus nerve is active during parasympathetic stimulation.
What Happens When We Have POTS?
When people have POTS from COVID or some other cause, the autonomic nervous system is confused. Doctors call this “dysautonomia.” That’s medicalese for a disorder of the autonomic nervous system.
Normally, if we stand up, our autonomic nervous system instantly adjusts to our change in position. Our heart speeds up a bit and blood vessels tighten. Blood flows to our brain more efficiently.
People with POTS often have their blood pressure drop when they stand up. That is what can lead to lightheadedness and/or dizziness. Some people may faint or fall down. Because this is autonomic, or, as some describe it, “automatic,” we have very little control over our heart rate or blood pressure. That’s why POTS has been hard to treat.
Stimulating the Tragus (ear flap) to Help POTS:
Here is an anatomical diagram of your outer ear so you can locate the tragus:
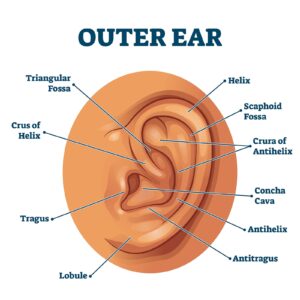
Outer ear anatomical structure educational scheme vector illustration. Labeled diagram with human sensory organ. Isolated closeup with triangular fossa, helix, tragus, lobule and concha cava location.
If that diagram is a bit daunting, just look at the photo of the woman’s ear at the top of the page. Do you see the small post earring? It is positioned right on the tragus.
Electrical Stimulation to Help POTS:
Enter some enterprising researchers at the University of Oklahoma Health Sciences Center. They were aware that if they stimulated the tragus (the little flap on the front of the ear) they might be able to stimulate the vagus nerve. This is called transcutaneous vagus nerve stimulation (tVNS).
The scientists describe their objectives to help POTS:
“We conducted a sham-controlled, double-blind, randomized clinical trial to examine the effect of tVNS on POTS over a 2-month period relative to sham stimulation.”
In other words, they used a very tiny electrical current to stimulate the tragus. They describe the electrical stimulation as “below discomfort threshold.” The control or sham stimulation involved the same equipment but the clip was attached to the earlobe instead of the tragus. The tragus connects to the vagus nerve, while the earlobe does not.
This was a small study. There were 12 POTS volunteers who got the tragus stimulation and 14 control subjects who had their ear lobes stimulated. Both groups received one hour of electrical stimulation daily over two months. The researchers measured the variability of heart rate using an electrocardiogram. They also did blood draws to detect inflammatory cytokines and autoantibodies.
The Envelope Please:
Did electrical stimulation help POTS? The authors write that :
“Postural tachycardia [rapid heart rate] was significantly less in the active arm [group that got stimulation of the tragus] compared with the sham arm [group that got simulation of the ear lobe]. Antiadrenergic autoantibodies and inflammatory cytokines were lower in the active arm compared with the sham arm at 2 months.”
The bottom line appears to be that electrical stimulation of the tragus can indeed help POTS.
Learn More About POTS and COVID:
We interviewed two expert guests about the complications of long COVID. In particular, we talked with Christina Kokorelis, MD, a member of the Johns Hopkins POTS program. She is a rehabilitation physician specializing in pediatric and adult postural orthostatic tachycardia syndrome (POTS), orthostatic intolerance and musculoskeletal rehabilitation. Here is a link to that interview.
In this condition, people may experience palpitations or lightheadedness as well as severe fatigue. When they stand, their heart rate may soar and they may become dizzy or faint.
Researchers at the University of Toledo have identified five inflammatory markers that suggest that POTS may have an autoimmune origin (Journal of Clinical Medicine, Feb. 6, 2021). Investigators in the UK are intrigued by reports that some long-COVID sufferers may have reduced symptoms after vaccination. They hypothesize that the shot may reset the immune system in some as yet undetermined way.
Your Turn:
Do you or someone you know have POTS? Please describe what it’s like. Have you tried anything to help POTS? What has worked and what hasn’t. Please share your experience in the comment section below.
Citations
- Stavrakis, S., et al, "Noninvasive Vagus Nerve Stimulation in Postural Tachycardia Syndrome: A Randomized Clinical Trial," JACC Clinical Electrophysiology, Nov. 10, 2023, doi: 10.1016/j.jacep.2023.10.015

