Most people have had a blood test for low-density lipoprotein cholesterol (LDL-C). It’s been dubbed “bad” cholesterol since the 1980s. Cardiologists write that “the prevalence of severely elevated LDL-C has declined, 1 in 17 adults still have LDL-C levels of 160 to 189…” (JAMA Cardiology, Dec. 1, 2023). That is about 6% of the population. Statins lower LDL cholesterol like magic, which is why a drug like atorvastatin is the most prescribed drug in the US. But there is another key risk factor for heart disease. It’s called lipoprotein(a) [Lp(a)]. Experts estimate that 20-30% of the population has elevated Lp(a) levels (Atherosclerosis, May, 2020). Why aren’t more people tested for Lp(a) levels?
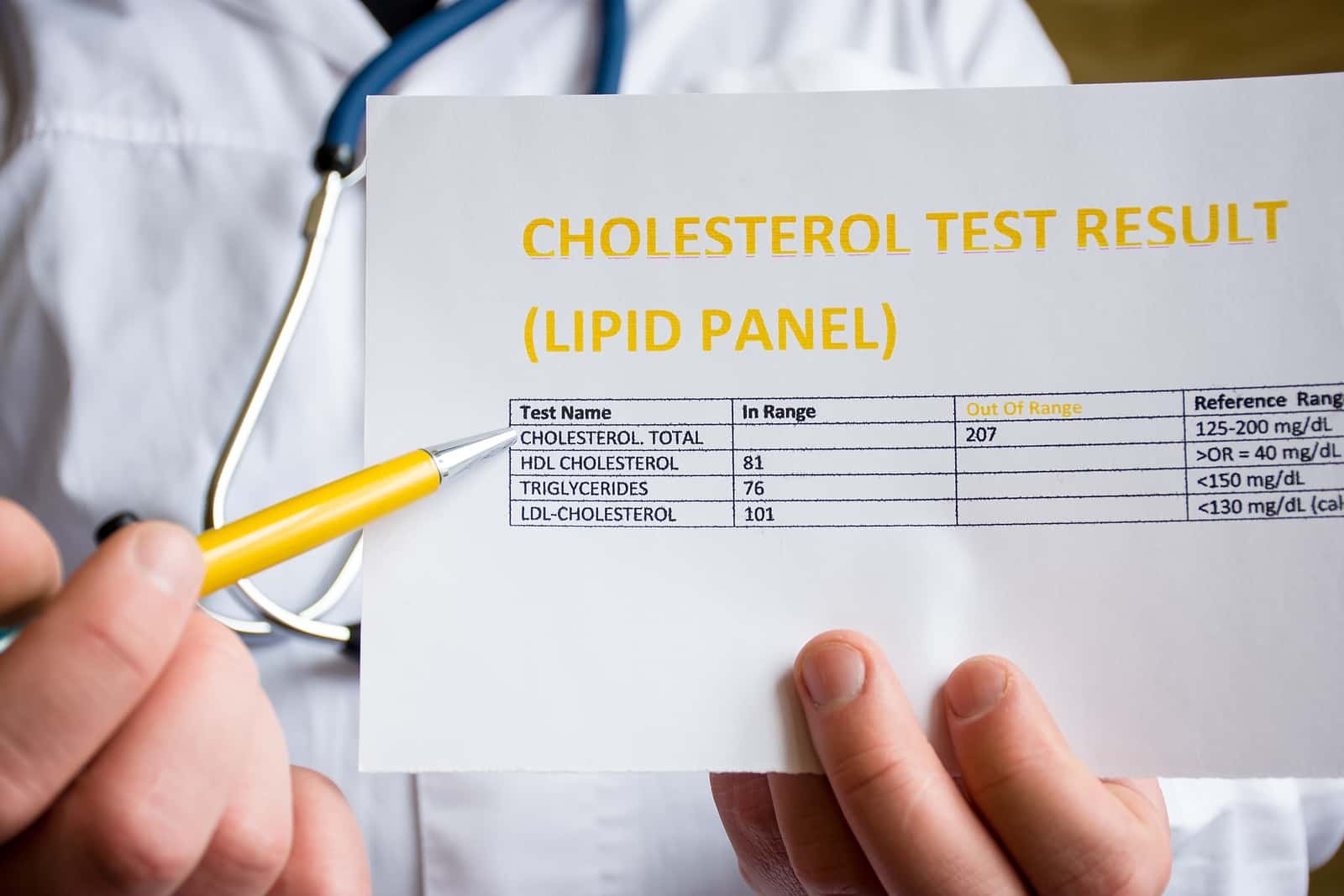
Has your doctor requested an Lp(a) test? If so, do you know what your results were? Many people know their LDL cholesterol levels. That’s because most cardiologists are committed to getting LDL cholesterol below 100 mg/dL.
Most people will only need to be tested for Lp(a) levels once. That’s because these numbers rarely change very much. If you have not been tested, you should be. We’ll tell you how you can do that with or without a doctor’s permission.
Why Should Anyone Be Tested for Lp(a) Levels?
Elevated levels of Lp(a) cause “atherosclerotic cardiovascular disease” abbreviated ASCVD). Please note that I said “cause.” This is not an association! Cardiologists know that this blood factor causes clogged arteries, heart attacks, strokes, and coronary heart disease deaths (Journal of the American College of Cardiology, April 2024).
A study also reveals that high Lp(a) levels also contribute to calcified heart valves and aortic valve stenosis (JAMA Cardiology, July 17, 2024). This is not good! When the aortic valve becomes calcified and reduces blood flow from the heart to the aorta, it causes all sorts of mischief. Symptoms may include chest pain, fatigue, dizziness, shortness of breath during exercise, heart palpitations and a heart murmur.
High Lp(a) levels are generally genetic. That means that if a grandfather, father, mother, uncle, aunt, or other close relative has had a heart attack or stroke, you should have your Lp(a) level measured. In fact, the National Lipid Association recommends that all adults should have their Lp(a) levels tested at least once. That’s because they generally do not vary very much over time. Once should be enough.
Why Don’t More Doctors Test Lp(a) Levels?
Great question. Here is what one reader shared:
Q. I read somewhere, possibly your column, that it’s advisable to have Lp(a) levels analyzed along with cholesterol at your annual wellness visit. This year my routine blood work came back with acceptable numbers for cholesterol, HDL and LDL. However, my small LDL particles were way too high.
My doctor said that most annual blood work does not include Lp(a). I wonder why not, since this lab value seems really important for predicting the risk for stroke or heart attack.
A. We don’t understand why many physicians seem reluctant to order a blood test for lipoprotein(a). This compound combines two troublemakers: LDL cholesterol and apolipoprotein(a). It can lead to calcification of aortic valves and clogged arteries. When there is a family history of heart disease, Lp(a) is often the culprit.
You can learn much more about Lp(a) and many other risk factors for cardiovascular disease in our eGuide to Cholesterol Control & Heart Health. This online resource can be found under the Health eGuides tab. In it you will discover ways to order these blood tests for yourself and some ways to improve your lab results.
Tired of Reading About Lp(a)?
Have you tired of reading about Lp(a) and heart disease? I do not blame you, but this risk factor has been ignored for so long that it is time to get caught up. A study published in the Journal of the American College of Cardiology (March 1, 2022) confirms that “…studies provide robust evidence that Lp(a) levels are causally associated with atherosclerotic cardiovascular (ASCVD) risk.” When coronary artery calcium scores (CAC) AND Lp(a) levels are elevated, the risk of heart attack or stroke goes up nearly five fold! Have you been tested for Lp(a) yet?
How Can You Be Tested for Lp(a)?
We received this question from a reader of our syndicated newspaper column:
Q. My father and his father had heart attacks at an early age. That is why I paid attention when I read that Lp(a) is an important risk factor for heart disease that runs in families. When I asked my doctor to order a blood test, she said that only a cardiologist can do that. Since I do not have one, what else can I do?
A. Any doctor could order a blood test for Lp(a). If your doctor is not cooperative, you could order this test yourself. Other readers report doing so online through HealthLabs.com or PrivateMDLabs.com at a cost of around $50-$60. Of course we think it would be best for your doctor to order the test so that she can help interpret the results.
In the past, some doctors have been reluctant to test for this blood lipid because there was no drug they could prescribe to lower it. That is beginning to change. Drugs for this purpose are now in clinical trials.
Another Readers Offers These Options for Getting Tested for Lp(a):
Q. Anyone having difficulty getting their doctor or insurance company to approve an Lp(a) blood test should be aware of several options to bypass those obstacles. A few web sites can be used to order this test and numerous other blood tests, with the person ordering the test paying out of pocket. One such web site is LifeExtension.com, which charges $39 for a test. You get a lab order you can take to a LabCorp or Quest Diagnostics office.
A. As I write this (but as there is a sale price of $29.25. We have zero relationship with LifeExtension or any laboratory!
Lipoprotein(a) is a significant risk factor for atherosclerosis and heart disease. It is estimated that one in five Americans has elevated levels of Lp(a), but only about one percent has been tested (New England Journal of Medicine, May 1, 2025).
You are correct that several websites offer consumers the option of ordering a test. In addition to LifeExtension.com, PrivateMDLabs.com and HealthLabs.com offer such tests. You can also order directly from Quest Diagnostics or Labcorp On Demand (ondemand.labcorp.com).
The ALPACA trial showed that the experimental drug lepodisiran can lower this blood lipid dramatically, by 40 to 90 percent, depending on dose (New England Journal of Medicine, May 1, 2025).
We don’t yet know whether lepodisiran or similar medications will be able to prevent heart attacks and strokes or aortic stenosis.
Have You Been Tested for Lp(a)?
Q. My wise family doctor in our home town in Texas began testing my Lp(a) in the early 2000s. It was around 21. My other lipids were off, so he prescribed a combination statin with niacin (Simcor). They eventually stopped making that medication.
We moved and I didn’t have my Lp(a) levels tested again until recently. It was 121! I couldn’t believe it.
I’ve been taking simvastatin for years. All my other lipid numbers are good. I’m perplexed about my high Lp(a) level. What will bring it back down?
A. Lipoprotein (a) is an important risk factor for heart disease. This single particle contains both LDL cholesterol and a sticky protein that helps Lp(a) form artery-clogging plaque.
Statins Do Not Lower Lp(a):
Unfortunately, statin drugs that lower cholesterol do not reduce Lp(a) levels. They may even raise it (BMC Cardiovascular Disorders, Nov. 8, 2022). That may explain why your Lp(a) went so high on simvastatin alone. Levels above 50 mg/dL increase the risk for serious cardiovascular problems.
The pharmaceutical industry is now developing drugs to manage Lp(a) levels. In the meantime, though, there are some dietary supplements that have a modest effect. Both niacin and L-carnitine bring this blood lipid down somewhat. A healthful low-carb diet can also reduce this risk factor (American Journal of Clinical Nutrition, Jan. 2022).
High Levels of Lp(a) Blamed for Heart Attack:
Q. I have followed a healthy lifestyle for decades and yet I still had a heart attack. It turns out that I inherited very high Lp(a) levels.
My doctors did not know much about this cardiac risk factor. They never included it in the standard lipid panels for cholesterol. I had to pay extra because Medicare does not cover the cost of the test.
For years now, I have been taking niacin along with vitamin C and the amino acids lysine and proline. At 78 years old, I am doing great! Why don’t doctors know about niacin for Lp(a)?
After Being Tested for Lp(a), Should You Take Niacin?
A. For years, doctors learned that lipoprotein (a), aka Lp(a), levels were inherited. They were told that neither drugs nor diet would be beneficial. Consequently, many saw no point in having patients tested for Lp(a).
Niacin was once a staple of coronary artery disease prevention, but statins replaced it. Niacin causes uncomfortable flushing when taken at doses that can lower cholesterol and Lp(a). Statins don’t produce that side effect. On the other hand, they tend to raise rather than lower Lp(a) levels (Pharmaceuticals, May 16, 2023).
Cardiologists are conducting clinical trials on new drugs designed to reduce Lp(a) levels. In the meantime, niacin can lower Lp(a) (Endocrine Practice, June 2023).
Readers who would like to learn more about cardiovascular risk factors, including Lp(a), will find useful information in our eGuide to Cholesterol Control and Heart Health.
Lp(a) Nastiness!
Research published in JAMA Network Open (Dec. 8, 2022) reveals another problem associated with elevated Lp(a) levels:
“In this large, retrospective cohort study using administrative data from a single center in France, we found that the Lp(a) level was independently associated with an increased incidence of major adverse limb events.”
What Are “Major Adverse Limb Events”?
Most people think about clogged arteries in the heart. That’s because they can lead to heart attacks. But arteries can become blocked all over the body. When the arteries in the legs become clogged, doctors call it peripheral artery disease (PAD).
The French scientists writing in JAMA Network Open (Dec. 8, 2022) describe the problem this way:
“Peripheral artery disease (PAD) is an atherosclerotic disease of the lower-limb arteries affecting more than 200 million people worldwide. Moreover, PAD remains underdiagnosed and untreated due to the asymptomatic onset of the disease. Patients with PAD can develop limb symptoms, ranging from claudication [pain in legs due to lack of oxygen] to critical limb-threatening ischemia [restricted blood flow], leading to a major adverse limb event, such as peripheral artery revascularization and lower-limb amputation.”
Major adverse limb events include amputations or strategies to open clogged blood vessels.
The Findings from France:
The latest research links high levels of Lp(a) to very serious lower limb vascular problems:
“In this cohort study, Lp(a) level was associated with an increased risk of lower-limb artery revascularization or major amputation among a large cohort of unselected hospitalized patients. Lipoprotein(a) needs to be considered to improve not only the cardiovascular risk but also the lower-limb vascular risk assessment.”
The authors suggest that people should be tested for Lp(a) levels!
Some doctors are not aware of the cardiovascular problems associated with elevated Lp(a) levels. Others resist ordering a blood test for reasons that we do not understand. This reader experienced just such a reaction from his doctor.
Sorry, You Can’t Be Tested for Lp(a)
Q. After reading your column about Lp(a) as a risk factor for heart disease, we asked my husband’s cardiologist for a blood test. He refused, saying that my husband was already on a statin and nothing else would be helpful. Is he right?
A. We recently interviewed one of the country’s leading experts on Lp(a), cardiologist Sotirios Tsimikas of the University of California, San Diego. He recommends that everyone be tested for Lp(a). Should you wish to listen to our interview, here is a link. We think this podcast is well worth your time to better understand this crucial cardiac topic better.
Show 1421: Is Lp(a) the Heart Risk No One Talks About? (March 16, 2025)
A strong family history of heart disease could indicate a genetic tendency for high levels of Lp(a). A cholesterol-lowering diet won’t affect this risk factor and statins actually raise it.
You can learn more about lipoprotein a and its role in both atherosclerosis and calcification of heart valves in our eGuide to Cholesterol Control and Heart Health. This online resource is available under the Health eGuides tab. You will also learn about ways to help lower Lp(a) levels with niacin, PCSK9 inhibitors and a low-carb diet.
Is There a Family History of Heart Disease or Stroke?
During your first meeting with any health professional, there will almost always be a question about family health history. In particular, doctors want to know if anyone in the family has had a heart attack or stroke. If so, it puts you at a greater risk for cardiovascular disease (CVD).
Cardiologists have known for decades that high levels of the blood lipid Lipoprotein (a) increase the likelihood for cardiovascular complications. Your genes largely determine how high this risk factor is.
That is to say if Grandpa, cousin Charlie or dad had high Lp(a) levels, there is a pretty good possibility you will too. If cardiovascular disease runs in the family, you should absolutely be tested for Lp(a) levels!
The MESA and Dallas Heart Study and Lp(a) Plus CAC:
The study published in the highly respected JACC (Journal of the American College of Cardiology, March 1, 2022) involved two big cohorts. MESA involves the study of 4,512 individuals in the Multi-Ethnic Study of Atherosclerosis trial. In addition, there were 2,078 people in the DHS (Dallas Heart Study). None of the subjects had signs of atherosclerosis or cardiovascular disease at the start of the study. The investigators followed their progress for more than 10 years.
Both groups were tested for Lp(a) levels and coronary artery calcium (CAC), a marker for atherosclerosis. The investigators wanted to determine the impact of Lp(a) alone, CAC score alone and the combined impact of high Lp(a) plus CAC upon atherosclerotic cardiovascular disease (ASCVD) risk.
And the Envelope Please:
The big take away from this impressive study was that participants who had both high Lp(a) levels and high coronary artery calcium scores:
…“had a nearly 5-fold increased ASCVD risk as compared with those with non-elevated Lp(a) and CAC = 0.”
Please hit the pause button. A 5-fold increased risk is crazy high! That is like a 500% increased risk of clogged arteries and cardiovascular disease. There are few things that increase the risk of serious disease to that extent. Please keep in mind that coronary artery calcium is not a risk factor per se; it is a measure of atherosclerosis. It is done with X-rays during a CT scan.
Comparing Lp(a) to LDL:
So, how does a high Lp(a) + high CAC score compare to elevated LDL cholesterol? Remember, cardiologists have been telling us that LDL is the primary problem in heart disease for a very long time.
A ten-year Danish study of more than 90,000 individuals reviewed the cardiac risk of people over 70 (The Lancet, Nov. 21, 2020). Those between 70 and 79 years old with high LDL scores around 193 mg/dl had an 82% higher risk of atherosclerotic cardiovascular disease and heart attacks. For older individuals over 80 years old, the risk nearly tripled.
We conclude that while LDL is important, Lp(a) poses a higher risk of atherosclerotic cardiovascular disease. Inexplicably, though, doctors have been ignoring it, more or less, for decades.
Why Haven’t You Been Tested for Lp(a)?
The authors of the study in the JACC (March 1, 2022) conclude that Lp(a) is independently associated with atherosclerotic cardiovascular disease. So is a high coronary artery calcium score. If both are elevated, the risk is scary high.
The authors conclude:
“Our novel findings indicate that elevated Lp(a) drives ASCVD [atherosclerotic cardiovascular disease] risk independent of the subclinical coronary atherosclerosis burden captured by CAC score. This is perhaps related to the unique pathways of inflammation and thrombosis that are triggered by elevated Lp(a) and oxidized phospholipid levels.”
With such an important risk factor, you would think that your doctor would have tested your Lp(a). Judging from comments on this website, though, that is rare. The authors of this important paper note that if levels are greater than 50 mg/dL, Lp(a) is a “risk-enhancing factor.”
What Are “Normal” Levels of Lp(a) and What are High Levels?
First, an apology. This gets way too complicated. For reasons that only a cardiologist can tell you, this important risk factor for heart disease has been underestimated. Don’t take my word for it. Here is what some smart clinician/researchers have to say in an article titled:
“Consensus and guidelines on lipoprotein(a) – Seeing the forest through the trees”
(Published in Current Opinion in Lipidology, Dec. 1, 2022)
“Since the contribution of high Lp(a) concentrations to global ASCVD [atherosclerotic cardiovascular disease] risk has been underestimated in the past, a clear recommendation to measure Lp(a) at least once in a person’s lifetime is imperative. Recent expert consensus recommendations provide clinicians with direction on how to manage the excess risk associated with elevated Lp(a) concentration by comprehensive and individualized management of modifiable ASCVD risk factors while awaiting the results of clinical trials of Lp(a) targeted therapies.”
So What’s Normal?
If you take the time to actually open the article above you will discover that there is no actual consensus about what is “normal” and what is “risky.” Recommendations are surprisingly variable. There is one more huge problem. Some laboratories measure Lp(a) in mg/dL (milligrams per deciliter) while others measure Lp(a) levels in nmol/L (nanomoles per liter).
We leave it to the individual laboratory and physician to interpret test results. In general, though, some researchers consider 30 to 50 mg/dL the “grey zone.” Below 30, no worries. Above 50, there is increased risk for atherosclerotic cardiovascular disease.
If the lab is measuring nmol/L, then “normal” is considered less than 75 nmol/L. When levels exceed 100 nmol/L, the person is considered at risk for heart disease. But there is some disagreement about the danger zone. The last time I checked, the American College of Cardiology/American Heart Association guidelines suggest that the risk threshold is reached when someone goes over 125 nmol/L.
What Happens When You Don’t Have a Hammer?
You have no doubt heard the phrase, “If all you have is a hammer, everything looks like a nail.” I suspect that cardiologists have rarely tested for Lp(a) because they don’t think they have a drug that will lower it.
Statins do not lower Lp(a). If anything, they raise it! We know that sounds like heresy, but that was the conclusion of a paper published in the European Heart Journal (June 21, 2020).
We suspect that meta-analysis made a lot of health professionals quite nervous. How could a drug that they have been prescribing for decades raise a serious risk factor for atherosclerotic cardiovascular disease? Read more about this contradiction at this link.
How to Lower Lp(a):
If you don’t have a hammer, it may be convenient to ignore the nails poking up through your floor. But eventually, they will cause damage. That’s why we think it is prudent to try to lower Lp(a).
Although most health professionals learned in medical school that they can’t lower Lp(a), that is not completely true. A study published in the American Journal of Clinical Nutrition (Jan. 2022) reveals that a low-carbohydrate diet can actually reduce levels of Lp(a). You can listen to the lead author, David Ludwig, MD, PhD, describe the results of this research at this link to our podcast.
When we spoke recently with Dr. Sam Tsimikas (March 16, 2025), he suggested that aspirin might be helpful for people with elevated Lp(a) levels.
An article in Current Atherosclerosis Reports, April 8, 2025 notes:
“Elevated Lp(a) is associated with increased risk for atherosclerotic cardiovascular disease (ASCVD), and there is currently a lack of targeted therapies for treating individuals with elevated Lp(a). The purpose of this review is to evaluate the current evidence for aspirin therapy for the primary prevention of ASCVD in individuals with elevated Lp(a).
“Prior studies demonstrated an association between aspirin use and a reduction in cardiovascular events among carriers of particular high-risk LPA single nucleotide polymorphisms. More recent studies have extended these findings by incorporating the more clinically available Lp(a) levels, observing an approximately 50% reduction in risk for coronary heart disease events and ASCVD mortality with aspirin use among individuals with Lp(a) > 50 mg/dL. There is growing evidence for a benefit with aspirin therapy in individuals with elevated Lp(a) without clinical ASCVD. The limitations of the available data must be acknowledged, and shared decision making should be used when discussing with patients, particularly when balancing potential bleeding risk.”
What About Niacin?
We wrote an article titled “Is Lp(a) the Best Kept Secret in Heart Disease?” some time ago.
In response, Fay posted this message in the comment section:
“You probably saved my life with this article. All 4 of my grandparents and both parents had a heart attack or stroke. I had never heard of Lp(a) and now I know to lower it. Robert Kowalski’s book from 2002 has the clue: The New 8-Week Cholesterol Cure. He quotes numerous reputable studies where SR (sustained release) niacin lowers Lp(a) as much as 33% to 50%. pp.137-141.”
That prompted us to dig up a copy of Robert Kowalski’s book, “The New 8-Week Cholesterol Cure.” We knew he was a big proponent of niacin.
We did not know that he was on to the problems with Lp(a) two decades ago:
“Levels of the blood fat triglycerides fall dramatically with niacin, far more so than with prescribed drugs…In an NIH–sponsored study, triglycerides fell an average of 52 percent. Regardless of percentage of improvement, niacin can bring triglycerides down to normal even if beginning levels are very high.
“The independent risk factor Lp(a) also succumbs to niacin, even though it responds to neither diet nor drugs. Lp(a) levels were down 35% when subjects were given niacin at the Oregon Health Sciences University. At the internationally renowned Karolinska Institute in Sweden, Lp(a) came down an average of 33 percent in all patients treated with niacin.”
What Happened to Niacin?
Doctors used to prescribe niacin. Statins pretty much put an end to that, though. All focus was on LDL cholesterol and statins lower it extremely well. Perhaps it’s time for doctors to rediscover niacin.
Learn More:
To learn more about niacin, check out this article we wrote a few years ago. It reveals some details about why doctors gave up on niacin. That may have been premature.
Learn about niacin side effects at this link. There are some things people can do to lower the likelihood of unpleasant symptoms. We do think a doctor should absolutely supervise when a patient takes niacin. There are slow-release prescription products that may reduce the risk of the niacin flush. And a doctor can monitor liver enzymes, which we think is important. Don’t forget to ask your doctor to have you tested for Lp(a).
Some practitioners prefer inexpensive immediate-release niacin instead of slow release products. That is what was tested in the Coronary Drug Project (JAMA, Jan. 27, 1975). These were patients who had already had a heart attack and were at high risk for another.
Plain old niacin for 5 to 6 years reduced the risk of another heart attack by 27%. That benefit lasted even after niacin had been stopped for six years. Immediate-release niacin also reduced the risk of strokes by 24%. Because flushing is a problem with immediate-release niacin, this approach is a go-low, go-slow process.
Learn more about Lp(a) and many ways to reduce cardiovascular risks in our eGuide to Cholesterol Control and Heart Health. It is available under the Health eGuides tab at this website. You can also listen to our free podcast interview with Dr. Tsimikas at this link. He is one of the world’s foremost authorities on Lp(a). Just click on the arrow inside the green circle under his photo.
A Favor, Please:
We would like to ask a small favor. If you think this article has value, please share it with family and friends. It’s easy; just scroll to the top of the page and click on the icons for email and social media. While you are at it, please encourage your contacts to subscribe to our free newsletter. That way they can keep up with the latest developments in the world of health. Here is a link to free subscriptions. You can also go ad-free while you are there or make a donation. Thank you for supporting our work. It keeps the newsletter and website moving forward.
Citations
- Mehta, A., et al, "Independent Association of Lipoprotein(a) and Coronary Artery Calcification With Atherosclerotic Cardiovascular Risk," Journal of the American College of Cardiology, March 1, 2022, doi: 10.1016/j.jacc.2021.11.058
- Zhu L et al, "Effect of an increase in Lp(a) following statin therapy on cardiovascular prognosis in secondary prevention population of coronary artery disease." BMC Cardiovascular Disorders, Nov. 8, 2022. DOI: 10.1186/s12872-022-02932-y
- Ebbeling CB et al, "Effects of a low-carbohydrate diet on insulin-resistant dyslipoproteinemia-a randomized controlled feeding trial." American Journal of Clinical Nutrition, Jan. 2022. DOI: 10.1093/ajcn/nqab287
- Koutsogianni AD et al, "Effects of lipid-modifying and other drugs on Lipoprotein(a) levels-Potent clinical implications." Pharmaceuticals, May 16, 2023. DOI: 10.3390/ph16050750
- Tsushima T et al, "Lipoprotein(a) and atherosclerotic cardiovascular disease, the impact of available lipid-lowering medications on Lipoprotein(a): An update on new therapies." Endocrine Practice, June 2023. DOI: 10.1016/j.eprac.2022.12.011
- Guedon, A. F., et al, "Association of Lipoprotein(a) Levels With Incidence of Major Adverse Limb Events," JAMA Network Open, Dec. 8, 2022, doi:10.1001/jamanetworkopen.2022.45720
- Wong, N.D., et al, "Lipoprotein(a) and Long-Term Cardiovascular Risk in a Multi-Ethnic Pooled Prospective Cohort," Journal of the American College of Cardiology, April, 2024, https://doi.org/10.1016/j.jacc.2024.02.031
- Arsenault, B.J., et al, "Lipoprotein(a) and Calcific Aortic Valve Stenosis Progression," JAMA Cardiology, July 17, 2024, doi:10.1001/jamacardio.2024.1882
- Razavi, A. and Bratia, H.S., "Role of Aspirin in Reducing Risk for Atherosclerotic Cardiovascular Disease in Individuals with Elevated Lipoprotein(a)," Current Atherosclerosis Reports, April 8, 2025, doi: 10.1007/s11883-025-01296-w

