Most cardiologists take it as absolute fact that cholesterol is a bad actor in the heart disease saga. They believe that LDL cholesterol in particular is responsible for causing clogged coronary arteries. Because statins lower LDL cholesterol very effectively, doctors conclude that such drugs prevent heart disease in most patients. Guidelines from the American College of Cardiology and the American Heart Association virtually require doctors to prescribe a statin-type cholesterol-lowering drug for most older individuals.
At last count, almost 50 million Americans take a statin. But if these drugs are so effective, why is heart disease still our # 1 killer? Statins have been prescribed in the US since 1987. One might have assumed that such drugs would have made a major dent in heart disease by now. You can read more about this puzzling contradiction at this link.
Clogged Coronary Arteries Despite Statins:
This man was not protected from cardiovascular disease:
Q. My father has been taking various statins for over 20 years. At first he was prescribed Zocor. Later he was told to take Lipitor. More recently his doctor had him on rosuvastatin.
Dad has had some aches and pains but has been able to tolerate these statins reasonably well. He has always maintained an active lifestyle. He walks daily and loves to play golf and tennis.
A few weeks ago he suffered some serious chest pain. When the cardiologists examined his coronary arteries they discovered that two were almost completely closed off (nearly 98% clogged) and another two were also in bad shape, though not totally blocked. They put stents in four arteries and he is now doing well.
What has us confused is how this could have happened. We thought statins were supposed to protect people from clogged coronary arteries and heart attacks. How could dad have ended up in such bad shape after all those years of a good diet and statin treatment?
A. We’re pleased to learn that your father is recovering well from this ordeal. That said, the question you raise is complicated and the answers remain controversial.
Another Statin Disappointment:
Another reader shares his personal story with clogged coronary arteries. It too challenges the LDL cholesterol theory of heart disease:
Q. I have never had high LDL cholesterol, but my doctors have prescribed statins for many years. I am currently taking atorvastatin.
Despite having taken these cholesterol-lowering drugs, I have coronary artery disease. I needed several angioplasties and stents placed after my heart attack. My cardiologist is now planning bypass surgery. In my case, lowering LDL cholesterol did not protect my heart.
A. Heart disease is complicated. Some people experience heart attacks even though their cholesterol levels are normal. Another blood lipid called lipoprotein(a), abbreviated Lp(a), is rarely tested but may contribute to clogged arteries. This risk factor usually runs in families. Somewhat surprisingly, statins may actually increase Lp(a) rather than lowering it.
Could Aspirin Be Helpful for People with High Lp(a) Levels?
This reader wants to prevent clogged coronary arteries despite high lipoprotein(a):
Q. I have very high Lp(a) levels. Your column has made me aware that this is a serious cardiovascular risk factor.
You recently wrote about a study regarding aspirin therapy for people with high Lp(a) levels. How much aspirin did volunteers in the study take?
A. High levels of Lp(a), are considered a major risk factor for coronary artery disease and heart valve damage. Many physicians have been reluctant to order tests for this blood lipid because they do not yet have an effective treatment.
Aspirin used to be recommended for heart disease prevention, even in people at relatively low risk for a heart attack. Now, though, cardiologists have determined that the possibility of dangerous bleeding outweighs the potential benefits in low-risk individuals.
A recent study found that aspirin therapy (100 mg per day) can reduce the risk of cardiovascular events among people who are at high risk due to elevated Lp(a) (European Heart Journal. Cardiovascular Pharmacotherapy, Feb. 8, 2025). Some cardiologists are also prescribing PCSK-9 inhibitors such as alirocumab (Praluent) and evolocumab (Repatha) for people like yourself with elevated Lp(a). These medications can lower levels of this risk factor a bit.
You may wish to listen to our podcast with one of the researchers who discovered the benefits of aspirin for patients with high Lp(a) levels. Here is a link to that interview with Dr. Sam Tsimikas.
To learn more about the pros and cons of statins and other ways to reduce heart risks, you may wish to read our eGuide to Cholesterol Control and Heart Health. This online resource is available under the Health eGuides tab.
The Cholesterol Hypothesis:
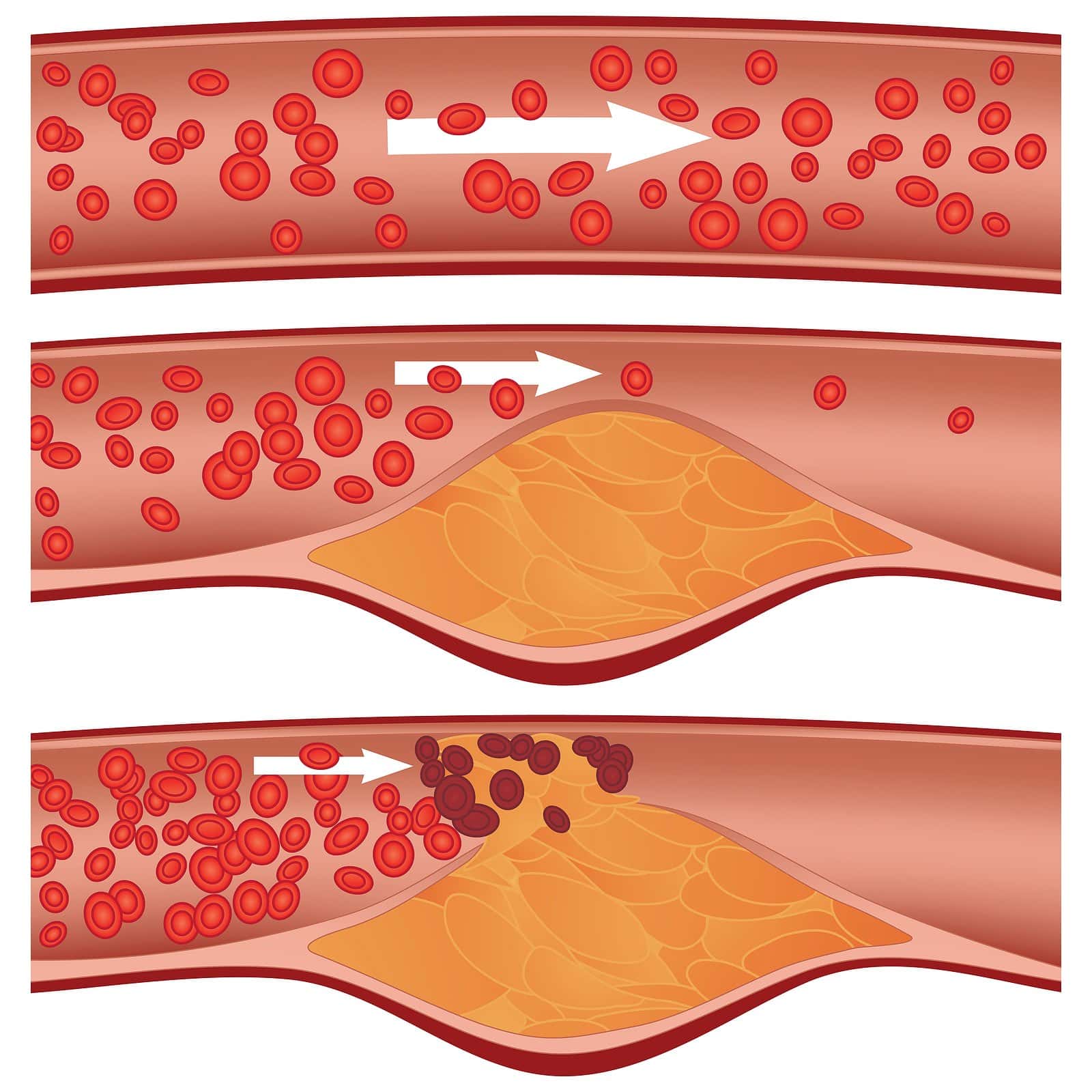
Ask most physicians what causes heart disease and heart attacks and they will tell you it’s primarily a cholesterol problem. Too much bad LDL cholesterol and/or too little good HDL cholesterol leads to plaque development and clogged coronary arteries. They point to numerous randomized controlled trials that show lowering LDL cholesterol reduces the risk of heart attacks, strokes and deaths from heart disease.
It seems like an open and shut case. That’s why tens of millions of Americans take statins such as atorvastatin (Lipitor), fluvastatin (lescol), lovastatin (Mevacor), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor).
How Good Are Statins at Preventing Clogged Coronary Arteries?
What is rarely mentioned in this discussion is how many people have to take a statin in order to prevent one heart attack. It’s a surprisingly large number. This is what is called the absolute risk reduction and most people zone out the minute we start talking about statistics. Please hang in there with us as we describe a major meta-analysis by statin enthusiasts (Lancet, Aug. 11, 2012).
These cardiologists and statisticians analyzed data from 27 clinical trials. Over 170,000 people participated in these studies. Cutting to the chase, here is what they found:
If 1,000 people took a statin instead of a placebo for five years there would have been 11 fewer “major vascular events.” Put another way, 5.2% of the people getting placebo experienced an “event” over the five year period whereas 4.1% of those on a statin had such an event. That represents a 1.1% improvement. Depending upon your perspective, this kind of risk reduction is either fabulous or modest. We offer no editorial opinion.
A Medical Heretic Analyzed the Data:
Dr. John Abramson, MD, MSc, has been a faculty member at Harvard Medical School for 25 years. He taught health-care policy. In his book, Sickening: How Big Pharma Broke American Health Care, he asked the following question:
“Does statin therapy provide a net benefit for people at low risk of cardiovascular disease?
To answer the question he “calculated the effect of statin therapy on overall mortality and on heart attacks and strokes in people whose risk of cardiovascular disease was less than 20 percent over the next ten years”:
“Our findings, published in the British Medical Journal in October, 2013, showed that statin therapy provides very little or no net benefit in this population:
“• no significant reduction in mortality (the overall risk of death)
• small (though statistically significant) reduction in the risk of nonfatal heart attack and stroke — 140 people with low risk (less than 20 percent five-year risk) must take a statin for five years to prevent one nonfatal event (NNT [number needed to treat] = 140)
• no reduction in serious adverse events (events serious enough to cause hospitalization) overall”
Many cardiologists reject Dr. Abramson’s calculations. They even tried to get him to retract his BMJ article. These pro-statin advocates were unsuccessful, however. After reanalyzing his data calculations, an independent analysis concluded that there were no grounds for retraction.
The Guidelines:
We can say that the American Heart Association and the American College of Cardiology have concluded that virtually every older person should be on a statin, regardless of risk factors. You could be a vegetarian and a marathon runner and it wouldn’t matter. The guidelines encourage many men over 56 to take a statin and women over 65 to be on such drugs.
The belief is that the lower the LDL cholesterol the better! In other words, Mother Nature messed up. She made a terrible mistake when she allowed the body to make LDL cholesterol.
The Cholesterol Hypothesis Under Fire:
Over the last couple of decades we have seen a number of health professionals resist the tidal wave of enthusiasm for a statin in every medicine cabinet. Most of these physicians have been general practitioners or internists. But there is now a cardiologist and lipid specialist who has joined their ranks.
Robert Dubroff, MD, was an associate professor of medicine in the Division of Cardiology at the University of New Mexico in Albuquerque, NM. He is a lipidologist, which means he understands cholesterol and its impact on blood vessels better than most health professionals. Dr. Dubroff recently retired and has written some intriguing articles. One is titled “Cholesterol Paradox: A Correlate Does Not a Surrogate Make” (Evidence Based Medicine, March, 2017).
A Cardiologist Challenges His Colleagues
Dr. Dubroff introduces his article this way:
“The global campaign to lower cholesterol by diet and drugs has failed to thwart the developing pandemic of coronary heart disease around the world. Some experts believe this failure is due to the explosive rise in obesity and diabetes, but it is equally plausible that the cholesterol hypothesis, which posits that lowering cholesterol prevents cardiovascular disease, is incorrect. The recently presented ACCELERATE trial dumbfounded many experts by failing to demonstrate any cardiovascular benefit of evacetrapib despite dramatically lowering low-density lipoprotein cholesterol and raising high-density lipoprotein cholesterol in high-risk patients with coronary disease.”
Dr. Dubroff refers to a randomized clinical trial called ACCELERATE. It undermined the very foundation of the cholesterol hypothesis of heart disease. That’s because the new drug evacetrapib was just about the perfect medicine. It lowered “bad” LDL cholesterol 37% and also raised “good” HDL cholesterol by 130%. No single drug has ever accomplished such impressive changes in the directions most cardiologists strive for.
The trouble was that despite such stellar numbers there was no benefit in terms of things patients care about. The drug did not reduce cardiovascular events or reduce deaths in high-risk patients.
More Bad News for the Cholesterol Theory & Clogged Coronary Arteries:
Dr. Dubroff also points out that:
“Many experts cite numerous RCTs [randomized controlled trials] of statins in support of the cholesterol hypothesis, but we should not ignore the dozens of cholesterol-lowering trials that do not…Even when researchers demonstrate a statin mortality benefit, the findings are underwhelming. A recent analysis concluded that statins would only postpone death by a median of 3.1 and 4.2 days for primary and secondary prevention, respectively.”
That was after years of statin use. For example, the famous 4S study produced survival gains of 27 days after 5.8 years of simvastatin therapy (BMJ Open, Sept. 24, 2015). That extra month of life was in very high-risk patients who either had already experienced a heart attack or were suffering severe symptoms of heart disease. In trials where people were at lower risk of a heart attack, the life-extending potential of statins was substantially less than a month. That was even after years of treatment.
Other Medical Heretics Weigh In on LDL Cholesterol:
Mention the name Uffe Ravnskov, MD, PhD, to an American cardiologist and you will likely get a scowl. This Danish physician has perturbed drug companies and US cardiologists for years. Together with other colleagues, including cardiologist Michel de Lorgeril, Dr. Ravnskov has challenged the LDL cholesterol concept of heart disease.
One article in particular created a lot of consternation. It was published in the journal Expert Review of Clinical Pharmacology, Oct. 2018 and was titled:
“LDL-C [Cholesterol] Does Not Cause Cardiovascular Disease: A Comprehensive Review of the Current Literature”
Here are the conclusions:
“The idea that high cholesterol levels in the blood are the main cause of CVD [cardiovascular disease] is impossible because people with low levels become just as atherosclerotic as people with high levels and their risk of suffering from CVD is the same or higher. The cholesterol hypothesis has been kept alive for decades by reviewers who have used misleading statistics, excluded the results from unsuccessful trials and ignored numerous contradictory observations.
“In our analysis of three major reviews, that claim the cholesterol hypothesis is indisputable and that statin treatment is an effective and safe way to lower the risk of CVD, we have found that their statements are invalid, compromised by misleading statistics, excluding unsuccessful trials, minimizing the side effects of cholesterol lowering, and ignoring contradictory observations from independent investigators.”
Please keep in mind that most US cardiologists disagree with Dr. Ravnskov and his colleagues. We are not here to be arbiters of the cholesterol theory of heart disease or make medical recommendations. That is always between a patient and the prescribing physician.
What Does It All Mean?
Cholesterol remains a suspect in heart disease. That said, there are a great many other factors that can increase the risk for heart attacks and strokes. Diet and exercise are cornerstones for good health. An article in JAMA (March 7, 2017) suggested that almost half of the deaths from heart disease, stroke and type 2 diabetes are related to poor dietary habits.
You can also read our summary of the research at this link:
Statins Aren’t Magic Bullets to Prevent Clogged Coronary Arteries:
There are many people who benefit from statins. But as the person who shared the story at the top of this article pointed out, there are no guarantees that a statin will always prevent clogged coronary arteries.
No one should ever stop prescription medicine without medical supervision. These days many doctors have adopted the concept of shared decision making. That means that patients should participate in the process of deciding about their treatment program.
To help with that process, we have prepared a Guide to Cholesterol Control and Heart Health. It can be accessed from the Health Guide section of our website. It discusses the risk factor Lp(a) that is rarely mentioned when doctors call for a blood test. What do statins do to Lp(a) levels? You may be surprised.
Share your own statin story below in the comment section.
Citations
- Ravnskov, U., et al, "LDL-C does not cause cardiovascular disease: a comprehensive review of the current literature," Expert Review of Clinical Pharmacology, Oct. 2018, DOI: 10.1080/17512433.2018.1519391
- Yu, C., et al, "Polygenic risk, aspirin, and primary prevention of coronary artery disease," European Heart Journal. Cardiovascular Pharmacotherapy, Feb. 8, 2025, doi: 10.1093/ehjcvp/pvae085

