Atrial fibrillation (AFib or A-fib or AF) is the most common serious irregular heart rhythm. Some experts are calling this arrhythmia an epidemic (Journal of Geriatric Cardiology, March, 2017). That’s because as many as 6 million people have AFib now. The CDC estimates that by 2030 over 12 million Americans will be diagnosed with AFib. An alarming new study in Circulation: Arrhythmia and Electrophysiology (April 22, 2024) suggests that younger people are showing up with this heart rhythm irregularity. What is the best way to treat atrial fibrillation?
AFib (AF) in Younger People Is Alarming!
This heart arrhythmia has been thought to be far more common in older people, but new data published in Circulation: Arrhythmia and Electrophysiology suggests that almost one quarter of those diagnosed with AFib are under 65.
This study was conducted at the University of Pittsburgh and involved 67,000 patients. Younger people with atrial fibrillation were more likely to have risk factors such as diabetes, hypertension, COPD, chronic kidney disease and coronary artery disease.
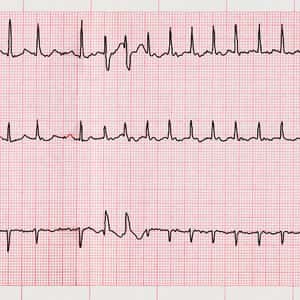
Symptoms of AFib may include heart palpitations, lightheadedness, fatigue, shortness of breath, irregular heartbeats and chest pain. Smart watches and credit-card-sized EKG devices are often capable of detecting this irregular heart rhythm.
That may partially explain why so many younger people are being diagnosed than in prior years. Their smart watch told them there was a problem and that got them to a clinic. I have another hypothesis. Medications can increase the risk for AFib.
Drug-Induced AF: The Elephant in the Room!
We suspect that most health professionals do not think about drug-induced atrial fibrillation. For example, high dose corticosteroids like prednisone can trigger AF. Millions of people get high doses of such steroids to treat rheumatoid arthritis, sinusitis, severe skin reactions and autoimmune disorders.
Nonsteroidal anti-inflammatory drugs (NSAIDs) can also bring on AFib. Very few people are warned that their favorite pain relievers (ibuprofen or naproxen) might trigger this arrhythmia.
Acid-suppressing drugs (proton-pump inhibitors) and diuretics can deplete the body of essential minerals. If magnesium or potassium levels go low, arrhythmias can occur.
You can learn more about drug-induced A-fib at this link.
It is important to treat this condition with anticoagulants or ablation therapy to prevent blood clots that could cause strokes.
Drugs or “Zapping” for AFib?
Cardiologists have been debating the best way to treat atrial fibrillation for years. Options include anti-arrhythmic drugs and anticoagulants vs. catheter ablation. The latter strategy involves the passage of a catheter into the heart. Heat or cold energy is then used to create a small scar in the heart muscle to prevent an electrical signal from triggering an abnormal rhythm.
The Downsides of Drugs:
A drug that has been frequently prescribed for AFib is amiodarone. This medication is tricky, though. It can cause a boatload of serious side effects. More important, though, is lack of FDA approval.
Here is what the FDA allows with amiodarone:
“Amiodarone hydrochloride tablets are indicated for the treatment of documented, life-threatening recurrent ventricular fibrillation and life-threatening recurrent hemodynamically unstable tachycardia in adults who have not responded to adequate doses of other available antiarrhythmics or when alternative agents cannot be tolerated.”
You can learn more about the dangers of amiodarone at this link:
Amiodarone Side Effects Can Be Life Threatening
Anticoagulants have their own challenges. Such drugs are a bit like walking a tightrope. On one side is the risk of blood clots. On the other is the risk of bleeding (hemorrhage). Successful treatment requires a careful balance between the two extremes.
So What is the Best Way to Treat Atrial Fibrillation?
A meta-analysis published in JAMA Cardiology (April 28, 2021) compared ablation therapy to antiarrhythmic drugs for overcoming paroxysmal AFib. The review included six randomized clinical trials with over 1200 patients.
Catheter ablation reduced arrhythmias 38 percent more than medications did. Even more important, it cut hospitalization by 68 percent more.
The authors conclude:
“In this meta-analysis of first-line therapy of patients with paroxysmal AF, compared with use of antiarrhythmic drugs, use of catheter ablation was associated with reductions in AF recurrence and hospitalizations, with no difference in major adverse events.”
The article offers this key point about the best way to treat atrial fibrillation:
“Meaning: Findings of this meta-analysis suggest the potential utility of catheter ablation as a first-line strategy in patients with paroxysmal atrial fibrillation compared with use of antiarrhythmic drugs.”
Please share your own experience with atrial fibrillation in the comment section below.
Citations
- Morillo CA et al, "Atrial fibrillation: the current epidemic." Journal of Geriatric Cardiology, March, 2017. doi: 10.11909/j.issn.1671-5411.2017.03.011
- Bhonsale, A., et al, "Mortality, Hospitalization, and Cardiac Interventions in Patients With Atrial Fibrillation Aged <65 Years," Circulation: Arrhythmia and Electrophysiology, April 22, 2024, https://doi.org/10.1161/CIRCEP.123.012143

