Life-Saving Lessons for COVID-19 from the Ebola Epidemic (Archive)
We are heartbroken that Dr. Paul Farmer, with whom we spoke in this episode, died suddenly on Feb. 21, 2022. He was a true hero. Our condolences to his family and colleagues. We are airing this interview in memoriam.
In 2014, an Ebola epidemic broke out in three countries of West Africa–Liberia, Guinea and Sierra Leone. Perhaps the first case was a toddler who became ill late in 2013, but it didn’t take long for the disease to spread. Medical care is rudimentary in the rural areas of these countries, and international organizations did not respond quickly. When they did, they focused primarily on containing the infection and preventing its spread rather than on providing care for its victims.
Lessons from the Ebola Epidemic:
Ebola is a virus that moves from one person to another. It causes fever, vomiting and diarrhea, which can lead to dehydration, shock and kidney damage. Oddly, the infection spread rapidly in some places but not in others. To understand why, we need to know more about the social and economic contexts of these places. Although Ebola has a fearsome reputation, with appropriate supportive care infected people usually survive. The trouble is that type of care is simply very scarce in the areas hardest hit by the epidemic.
A Lens on COVID-19:
Unlike Ebola, SARS-CoV-2 moves through the air with coughs, sneezes, talking or singing. However, there are some similarities. When a person infected with COVID-19 becomes ill, the best thing that the medical community can do for them is provide supportive care. No magic bullets stop the disease in its tracks, but intensive care makes a difference.
How does the previous Ebola epidemic in West Africa compare to what is happening with COVID-19 in the US and UK now? Healthcare systems in the US are being stretched to their breaking points much as they were in Sierra Leone, Guinea and Liberia.
Bringing the Lessons Home from the Ebola Epidemic:
Partners In Health has been working in Rwanda for decades. But responding to the Ebola epidemic was an enormous challenge. Now, PIH is sharing its expertise to help parts of the US confront COVID-19. What are they doing? How should this country strengthen its battered public health infrastructure to help overcome the pandemic and future outbreaks? Dr. Larry Brilliant has said outbreaks are inevitable; pandemics are optional. How could we make that statement true?
This Week’s Guest:
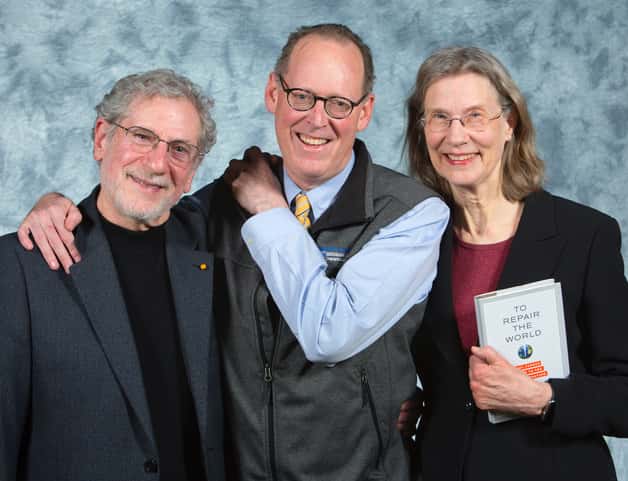
Paul Farmer, MD, PhD, was Kolokotrones University Professor and chair of the Department of Global Health and Social Medicine at Harvard Medical School, chief of the Division of Global Health Equity at Brigham and Women’s Hospital in Boston, and Co-founder and chief strategist of Partners In Health (PIH). Dr. Farmer and his colleagues pioneered novel, community-based treatment strategies that demonstrate the delivery of high-quality health care in resource-poor settings.
Dr. Farmer was the author of several books, including Partner to the Poor, Haiti After the Earthquake, Pathologies of Power, and To Repair the World. His latest is Fevers, Feuds, and Diamonds: Ebola and the Ravages of History.
Listen to the Podcast:
The podcast of this program is now available following its broadcast on January 30, 2021. The show can be streamed online from this site and podcasts can be downloaded for free.
Obituaries:
We offer links to these obituaries of our hero:
From The New York Times
From The Atlantic

