Have you ever experienced a bad bout of diarrhea after finishing a course of antibiotics? This reaction is not uncommon. Now, researchers are beginning to recognize that often this problem is caused by Clostridioides difficile, that is, C. diff due to antibiotics. Because it is due to bacterial overgrowth, doctors sometimes try to treat it with other antibiotics. But that doesn’t always work. Now the FDA is considering a novel treatment–bacteria!
Can a Bacterial Cocktail Cure C. Diff Due to Antibiotics?
C. diff is hard to eradicate, even with strong antibiotics. It can cause devastating diarrhea, abdominal cramping and dehydration among other problems. Some people with recurrent bouts have died as a result. Sometimes doctors treat stubborn cases with a fecal microbiota transplant.
The FDA has granted fast track status to a unique cocktail of nontoxic bacteria under the name VE303. This live biotherapeutic product contains 5 strains of nontoxic clostridia bacteria. A randomized controlled trial published in JAMA concluded that VE303 prevented C. diff recurrences better than placebo (JAMA, April 15, 2023). Among 79 patients with recurrent C. diff, 45% on the placebo had a recurrence during the trial. In comparison, not quite 14% of those getting a high dose of VE303 experienced a recurrence. The FDA will expect additional studies confirming these results before it approves the product.
It is certainly promising to learn that there may be a treatment on the way. Can people use probiotics that are currently available to prevent C. diff, rather than waiting for the new product?
Could a Common Probiotic Help Against C. Diff?
Q. My elderly mother had C. diff, as did a dear friend of mine who had been hospitalized. Both were treated with vancomycin, but the C. diff would return with debilitating diarrhea.
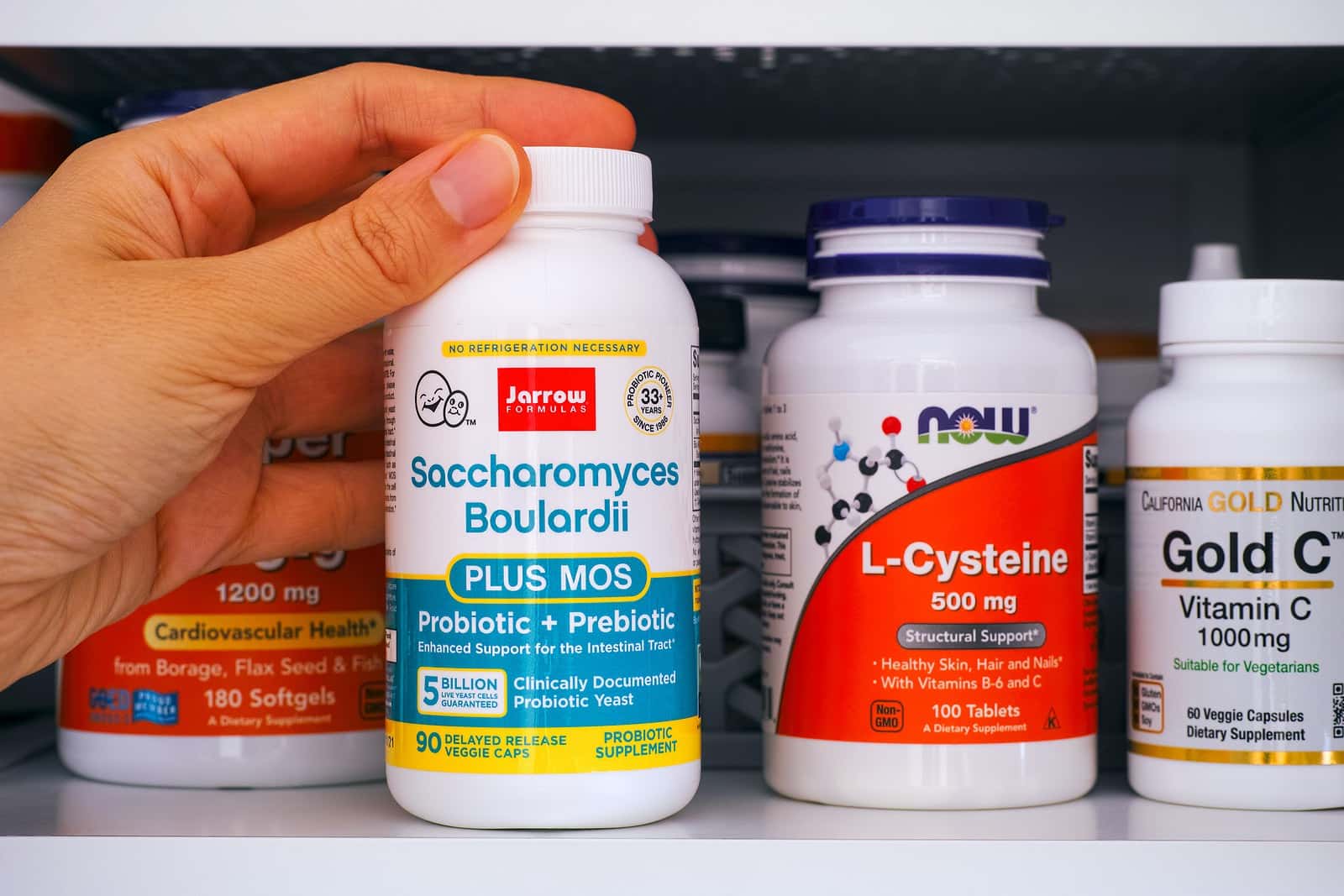
I looked online for information about this infection. When I read that the probiotic Saccharomyces boulardii might be helpful, both my mother and my friend started taking it. I was amazed how well it worked.
A. Clostridium difficile (now termed Clostridioides difficile) infection can occur after antibiotic treatment. If the antibiotics kill off beneficial bacteria, C. diff proliferates and causes terrible diarrhea. It can be very difficult to treat.
A Cochrane review found that probiotics such as the one you provided can prevent diarrhea due to C. diff (Cochrane Database of Systematic Reviews, Dec. 19, 2017).
In fact, the impartial volunteer physicians conducting this analysis concluded:
“The short-term use of probiotics appears to be safe and effective when used along with antibiotics in patients who are not immunocompromised or severely debilitated.”
Even more recently, scientists have confirmed that the kind of probiotic you recommended is effective for treating C. diff (Advances in Experimental Medicine and Biology, 2024).
C. Diff Due to Antibiotics:
Q. My mother, my father, my grandmother and my mother-in-law all developed an uncontrollable, nasty diarrhea caused by Clostridium difficile after taking antibiotics (especially Cipro). C. diff is the name of bacteria that live in the gut with other normal bacteria, causing no problems when a person is healthy. However, when a person takes a strong antibiotic for an infection, the medicine kills the normal bacteria in the gut and the C. diff remains. It no longer has any competition from normal flora. When it grows, it produces a toxin that causes severe diarrhea.
A pharmacist recommended taking the probiotic Saccharomyces boulardii whenever we are on an antibiotic. This yeast is not susceptible to most antibiotics. It helps keep C. diff in check and prevents diarrhea. Do you agree that this is a good protocol? It seems to work for my family.
The Evidence on Probiotics:
A. Scientists don’t all agree on whether or not probiotics can help prevent C. diff due to antibiotics. Saccharomyces boulardii is a probiotic that has been recommended widely to help counteract antibiotic-associated diarrhea. In fact, research demonstrates that when hospitalized patients take S. boulardii they are less likely to develop diarrhea after antibiotics (Clinical Infectious Diseases, June 23, 2020; European Journal of Clinical Microbiology & Infectious Diseases, Aug. 2018).
Because S. boulardii is a yeast rather than a bacteria, antibiotics don’t kill it (Current Microbiology, Sep. 2020). Consequently, it is useful for people taking antibiotics. They don’t have to worry that the medicine killing off the pathogens will also kill the probiotic bacteria such as Lactobacillus they take at the same time. Bacterial probiotic strains can be helpful in other situations, however.
Citations
- Louie T et al, "VE303, a defined bacterial consortium, for prevention of recurrent Clostridioides difficile infection: A randomized clinical trial." JAMA, April 15, 2023. doi:10.1001/jama.2023.4314
- Goldenberg JZ et al, "Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children." Cochrane Database of Systematic Reviews, Dec. 19, 2017. DOI: 10.1002/14651858.CD006095.pub4
- Levy EI et al, "Clostridioides difficile infections: Prevention and treatment strategies." Advances in Experimental Medicine and Biology, 2024. DOI: 10.1007/978-3-031-58572-2_11
- Wombwell E et al, "The effect of Saccharomyces boulardii primary prevention on risk of Hospital Onset Clostridioides difficile infection in hospitalized patients administered antibiotics frequently associated with Clostridioides difficile infection." Clinical Infectious Diseases, June 23, 2020. DOI: 10.1093/cid/ciaa808
- Carstensen JW et al, "Use of prophylactic Saccharomyces boulardii to prevent Clostridium difficile infection in hospitalized patients: a controlled prospective intervention study." European Journal of Clinical Microbiology & Infectious Diseases, Aug. 2018. DOI: 10.1007/s10096-018-3267-x
- Kaźmierczak-Siedlecka K et al, "Saccharomyces boulardii CNCM I-745: A non-bacterial microorganism used as probiotic agent in supporting treatment of selected diseases." Current Microbiology, Sep. 2020. DOI: 10.1007/s00284-020-02053-9

