Atrial fibrillation (AFib or AF) is a big hairy heart deal. For decades, doctors believed it affected more than 3 million American Adults. Then the CDC suggested that as many as six million Americans suffered from this irregular heart rhythm. A new study of 30 million people receiving healthcare in California indicates that almost 5% of the US population actually has AFib. That amounts to 10.5 million US adults. The study was published in the Journal of the American College of Cardiology, Sept. 11, 2024. Yikes! What is going on?
Atrial Fibrillation Is Going Up Fast!
A decade ago cardiologists were estimating that cases of atrial fibrillation would double to 12 million people by 2030 (American Journal of Cardiology, Oct. 15, 2013). We are almost there and we are still well-short of 2030.
The authors of the new research point out that (Journal of the American College of Cardiology, Sept. 11, 2024):
“The number of patients with a diagnosis of AF in California has markedly increased over time.
“Even earlier reports of AF described before the contemporary period suggested that AF rates were rising, and investigations outside of the United States have reported similar trends. This has been attributed to a combination of factors, including population growth and aging, increasing prevalence of risk factors for AF in many populations, improved survival, and enhanced AF detection.”
Conclusions:
“The prevalence of AF has risen substantially in recent years, exceeding prior predictions pertinent to the current era. We estimate that there were ∼10.55 million adults with diagnosed AF in the United States in 2019. Given the adverse consequences and considerable health care utilization associated with the disease, this rising prevalence calls for greater resource allocation and more efficient prevention and treatment strategies to curb the increasing burden of AF in the United States.”
A older review in the Mayo Clinic Proceedings (December, 2016) also concludes:
“Atrial fibrillation (AF) is the most common sustained arrhythmia in adults, and its prevalence is expected to increase 3-fold in the next 3 decades. Experts now characterize these epidemiological trends as an AF epidemic.”
What’s Causing the AF Epidemic?
The most common answer is age. Older people are more susceptible to atrial fibrillation than younger people. Populations are aging. But that doesn’t really tell us what’s behind this fast growing epidemic.
Some hypothesize that it’s due to increases in blood pressure. But the data suggest that rates of hypertension have stabilized due in large part to improved blood pressure control (JAMA, May 26, 2010). Therefore one might argue that blood pressure is probably not responsible for the dramatic increase in AF incidence.
Some experts suggest that obesity and diabetes could be contributing risk factors (European Heart Journal. Cardiovascular Pharmacotherapy, Apr. 2016). It is not clear, though, that weight reduction and tight glucose control could reverse the AF epidemic. Other risk factors that have been proposed include heart failure, hyperthyroidism and kidney disease.
AFib Anomalies:
Experts cannot explain the following:
- White people are more likely to develop atrial fibrillation than African Americans and Latinos. That’s despite the fact that African Americans and Latinos are more likely to suffer from overweight, diabetes and hypertension.
- There is twice as much AFib in developed regions compared to developing countries (Circulation, Feb. 24, 2014). Australia, Western Europe, Scandinavia and the United States have much higher rates of this arrhythmia than countries like Brazil, China, Colombia, India, Mexico, Peru or Russia.
Why We Should Care About AFib!
Atrial fibrillation has become a huge public health problem. That’s because this arrhythmia greatly increases the risk of hospitalization, stroke and death. The annual medical cost of AFib in the U.S. could be as high as $26 billion! It is estimated that each American with AFib could run up a tab of $8,705 a year (Circulation. Cardiovascular Quality and Outcomes, May, 2011). That is a budget buster for individuals, insurance companies and tax payers (think skyrocketing Medicare costs).
This does not take into account human suffering. People with AFib can suffer life-threatening complications because of this irregular heart rhythm. More about that below. And the treatments are not benign. Drugs to control this arrhythmia have some pretty serious side effects. You can learn more about the hazards of amiodarone at this link. And anticoagulants like apixaban (Eliquis), dabigatran (Pradaxa), rivaroxaban (Xarelto) and warfarin (Coumadin) carry their own risks. More about that at this link.
What is Atrial Fibrillation?
AFib happens when the upper chambers of the heart don’t function properly. Blood can pool, allowing clots to form. These blood clots can then be pumped to the brain and cause severe damage.
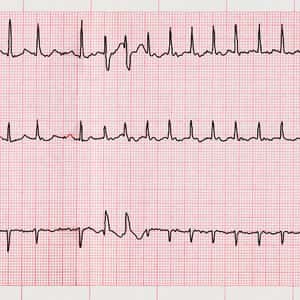
Symptoms of AFib include shortness of breath, fatigue, lightheadedness, chest pain and palpitations (a feeling of pounding or fluttering in the chest). An electrocardiogram is used to diagnose this arrhythmia. An app, Kardia from AliveCor, can be installed on a smart phone to detect this irregular heart rhythm.
Drug-Induced AF: The Elephant in the Room
One risk factor that is often overlooked when AFib is discussed in the medical literature is medication. A surprising number of drugs may increase the chance of developing atrial fibrillation.
Cortisone-type Drugs:
Millions of people take high doses of corticosteroids such as prednisone for a variety of health conditions including asthma, sinusitis, COPD, severe skin reactions and rheumatoid arthritis. A study in JAMA Internal Medicine (May 8, 2006) concluded that people taking cortisone-type drugs were significantly more likely to develop AFib. The researchers encourage physicians to monitor people for abnormal heart rhythms while receiving corticosteroids.
NSAIDs and AFIB:
Other drugs that can also trigger this AFib include the nonsteroidal anti-inflammatory drugs (NSAIDs) that so many people take to relieve pain. Drugs like diclofenac, ibuprofen and naproxen increase the risk of developing AFib by up to 80 percent (BMJ Open, Apr. 8, 2014). According to the senior author of this Dutch study, Dr. Bruno H. Stricker:
“I would really strongly advise that older people be very careful with using these drugs. They don’t do anything except relieve pain. Pain is a nuisance, but dying is a nuisance, too.”
Mineral Depletion and AFib:
People who take NSAID-type pain relievers are at greater risk for heartburn and stomach ulcers. They may turn to acid-suppressing drugs such as esomeprazole (Nexium), lansoprazole (Prevacid) and omeprazole (Prilosec) for relief. Such proton pump inhibitors can deplete the body of magnesium if they are taken for long periods of time. When magnesium levels drop, atrial fibrillation is a potentially serious complication.
Diuretics used to lower blood pressure may also lower magnesium and potassium levels. This could also put some people at risk for atrial fibrillation. This is a classic catch-22. If hypertension increases the risk of AF, the appropriate treatment would be blood pressure lowering drugs. But the most commonly prescribed drugs, diuretics, might actually increase the risk of AF due to depletion of key electrolytes.
Other Drugs and AFib:
According to the Journal of the American College of Cardiology (Dec. 2004), other drugs that have been linked to AFib include antidepressants (fluoxetine, tranylcypromine and trazodone), an antipsychotic (clozapine), migraine medicine, (sumatriptan) and medication for erectile dysfunction (sildenafil). Certain cancer drugs and some medications used to treat heart problems may also precipitate AFib (Kaakeh et al, Drugs, Aug. 20, 2012).
Drugs that make the heart beat faster can make a person more susceptible to AFib, but so can drugs that slow the heart rate. Turkish doctors reported on a person whose AFib was triggered by the combination of beta-blockers and diltiazem (Altunbas et al, Journal of Atrial Fibrillation, Oct. 31, 2016).
The Take Home Message:
When cardiologists are consulted because a patient has atrial fibrillation, they frequently prescribe anticoagulants or antiarrhythmics. They may also recommend an ablation procedure to try to correct the underlying arrhythmia. These are valuable treatments, but there are risks associated with surgery as well as drug treatment.
People on anticoagulants walk a tightrope. On one side is the risk of a blood clot that could cause a thrombotic stroke. On the other side is excess bleeding that could cause a hemorrhagic stroke. This is a very careful balancing act.
Perhaps doctors should start any evaluation of atrial fibrillation by carefully reviewing the patient’s list of medications. Drugs that can predispose a person to AFib should be reviewed very carefully. And perhaps patients should not assume that medications like NSAIDS that they can buy over the counter are completely safe.
Share your own experience with atrial fibrillation in the comment section below.
Citations
- Noubiap, J.J., et al, "Minimum National Prevalence of Diagnosed Atrial Fibrillation Inferred From California Acute Care Facilities," Journal of the American College of Cardiology, Sept. 11, 2024, https://doi.org/10.1016/j.jacc.2024.07.014

