The next time you get a prescription from your physician that says “take once a day,” stop! Do not accept such a vague instruction. Ask the prescriber what precisely that means and follow up with the pharmacist. Ambiguous prescriptions are dangerous. Should you be taking your medicine in the morning or in the evening? Timing matters for many medications. More importantly, food and drug interactions are common and can be life threatening.
What You Need to Know:
Find out if you should be taking your medicine with meals or on an empty stomach, and if there are any specific foods or beverages that might interfere with its proper action. A reader recently asked what seemed like a simple question:
Q. If a medication is supposed to be taken before meals, how much time before meals does that mean?
A. “Before meals” is much too ambiguous to be useful. If your doctor meant for you to take the medicine on an empty stomach, that would be at least one hour before eating or two hours after finishing a meal.
If your doctor meant “take with food,” that would be at mealtime. Have your doctor or pharmacist specify exactly what was intended.
Why the FDA has Let Doctors and Patients Down:
You would assume that physicians would have easy access to dosing information when it comes to the medicines they prescribe. How you take your pills can have a profound impact on how well they get into your bloodstream and circulate through your body.
Food and Drug interaction data is harder to obtain than you might imagine. Pharmaceutical companies try to keep things simple. During clinical testing that may mean giving the drugs in the same way to everyone in a laboratory setting. It’s easier to have subjects swallow pills on an empty stomach. It cuts down on variables like fat, which can influence drug absorption.
Someone who has scrambled eggs and sausage, buttered toast and coffee may react differently to a medicine from someone who has low-fat yogurt or oatmeal. Esomeprazole (Nexium) is less well absorbed when taken close to a high fat meal (Sostek, M.B., et al., British Journal of Clinical Pharmacology, Sept., 2007).
Acetaminophen Liver Toxicity and Food:
People take acetaminophen (Tylenol, etc.) for granted. It is found in hundreds of OTC pain relievers and cold remedies. We have known for decades that this drug can be tough on the liver. Take too much and serious liver toxicity can be a complication.
What most people do not know, though, is that when acetaminophen is taken in a fasted state it can increase the risk of liver damage (Whitcomb, D.C., et al., JAMA, Dec. 21, 1994). You might thing this piece of arcane pharmacology is irrelevant to you. You could be dead wrong!
When you have the flu, are suffering from severe pain or a terrible headache, you might not feel like eating. When we have the flu we stop eating for a couple of days. But if we are also suffering from aches and pains and a fever, we might take a fair amount of acetaminophen. That combination has been shown to toxic to the liver. A study in mice confirms this old observation (Antoine, D.J., et al., Molecular Medicine, Nov-Dec, 2010).
Other Examples Food and Drug Interactions:
Milk and other dairy products seem perfectly harmless for people who are not lactose intolerant. But if you are taking an antibiotic such as ciprofloxacin (Cipro) or norfloxacin (Noroxin) absorption may be reduced by 50 percent or more if swallowed in proximity to dairy products. That could sabotage the effectiveness of the antibiotic.
The laxative bisacodyl is found in Ducolax, Ex-Lax Ultra and Fleet Stimulant Laxative. Such products are coated to keep them from dissolving in the acid environment of the stomach. They are supposed to work in the lower intestines.
Taking bisacodyl with milk or yogurt can cause early, inappropriate absorption. The could lead to symptoms such as nausea, stomach cramps, diarrhea and a big bellyache.
Levothyroxine and Food and Drug Interactions:
The most widely prescribed drug in America is levothyroxine. Over 120 million prescriptions are dispensed and that does not include the brand name Synthroid. Absorption of this thyroid hormone (T4) is surprisingly variable. According to the FDA:
“Absorption of orally administered T4 from the gastrointestinal (GI) tract ranges from 40% to 80%.”
Let that sink in for a moment. That is a huge variation. Imagine if the fuel pumps at your favorite gas station delivered anywhere from 40% to 80% of the gas you purchased. You would be infuriated to learn that there was so much variability. But wait, it gets more complicated. The FDA goes on to say:
“T4 absorption is increased by fasting…Dietary fiber decreases bioavailability of T4. Absorption may also decrease with age. In addition, many drugs and foods affect T4 absorption…
“Consumption of certain foods may affect levothyroxine absorption thereby necessitating adjustments in dosing. Soybean flour, cotton seed meal, walnuts, and dietary fiber may bind and decrease the absorption of levothyroxine sodium from the GI tract.”
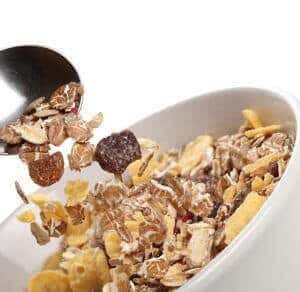
Many people may not be able to get up an hour before breakfast on a busy workday to swallow their levothyroxine pill on an empty stomach. If a woman has oatmeal or granola plus some walnuts, she may not get adequate amounts of T4 to do her much good if she takes her thyroid supplement within half an hour of breakfast.
The Bottom Line on Food and Drug Interactions:
Always ask your prescriber and pharmacist for specific information about how to take medicine. “Before meals” is a totally unacceptable instruction. If you are supposed to swallow your pills on an empty stomach, that generally means at least one hour before eating or two hours afterward. Never accept a prescription that just says take once a day. Find out what that means exactly with regard to food or beverages.
Ask about specific food and drug interactions. In some cases, such as T4, it matters whether you eat a high-fiber meal. In other situations fat makes a difference. Grapefruit can pose a problem for dozens of medications. So can pudding or salad dressing.
To help you sort out this confusing situation we offer our free Drug Safety Questionnaire which you can download, copy and give to your doctors and pharmacist. They should be encouraged to fill it out so you will have detailed instructions on food and drug interactions. We also offer our free Guides to Alcohol, Nutrient and Food Interactions with more information on why this is such an important topic.
To help you avoid other prescribing and dispensing errors we offer our book: Top Screwups Doctors Make and How to Avoid Them:

