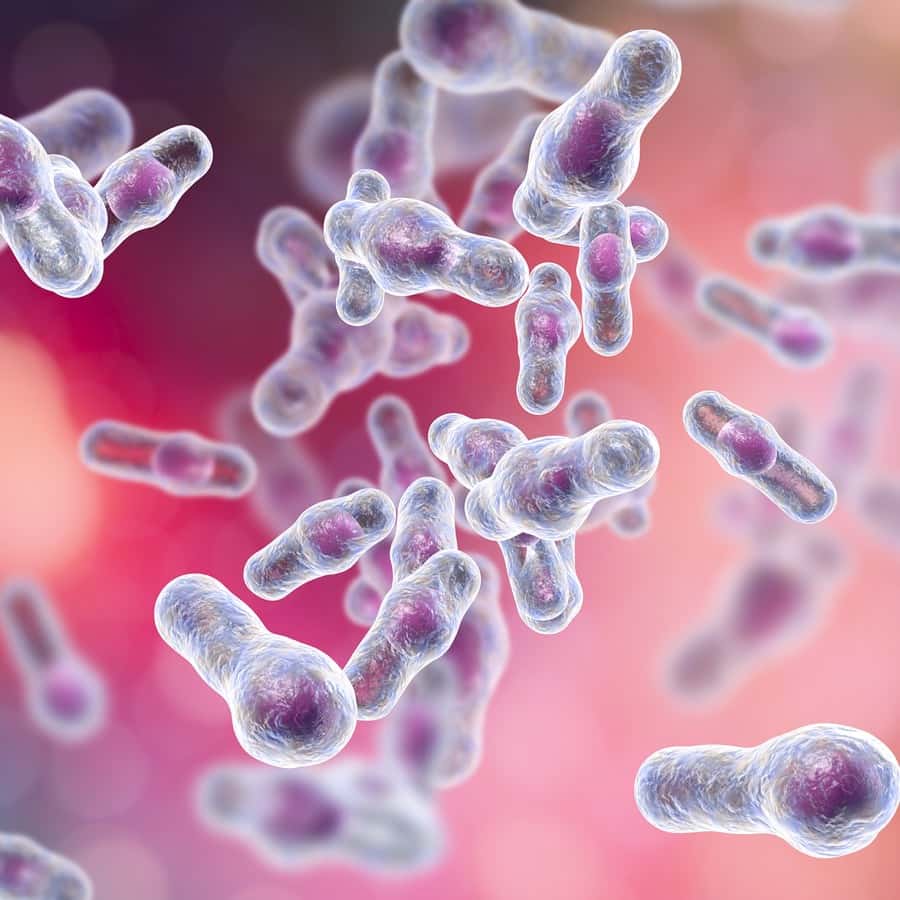
C diff infections were once thought to be limited to hospitals, nursing homes and other health care facilities. Such infections can cause severe, occasionally life-threatening diarrhea. Intestinal infections with Clostridioides difficile are hard to treat because they tend to come back even after a person has completed a full course of antibiotics.
What Do You Know About C Diff?
The bacterium was discovered as part of the normal intestinal flora in 1935. Shortly after that, doctors found that some patients developed serious diarrhea in reaction to antibiotic treatment. It wasn’t until 1974 that scientists identified C diff overgrowth as the culprit in such cases.
Clostridioides bacteria can make spores that resist disinfection, making it a persistent problem in nursing homes and hospitals. Anything that moves from room to room, such as a wheelchair, can contribute to its spread (American Journal of Infection Control, April 2019). Now, however, C diff is causing trouble everywhere.
C Diff Infections in the Community:
The CDC counted approximately 350,000 C diff infections in 2011. Nearly half of them had no connection to hospitals, and more than one third were not preceded by antibiotic use. In 2017, California researchers found that ten percent of emergency room patients with diarrhea had C diff.
Researchers speculate that changes in digestive microbiota may be making us more susceptible to this opportunistic infection. Presumably, it might be possible to reverse these changes with a diet full of fiber-rich vegetables and beans. That would mean eating less processed food.
Another potential culprit is the widespread use of acid-suppressing drugs such as esomeprazole, lansoprazole or omeprazole. People who take such heartburn medicine (think Nexium, Prevacid or Prilosec) on a regular basis are at increased risk for C. diff.
Treating C Diff Infections:
The usual treatment of C diff is with antibiotics. However, when it recurs, doctors are turning more frequently to fecal matter transplants (Frontiers in Microbiology, Nov. 2, 2018). This procedure allows for the re-establishment of a healthy microbial balance in the large intestine. To learn more about this procedure, you may wish to listen to our interview with Dr. Michael Bretthauer, President of the Frontier Science Foundation in Brookline, MA. It is Show 1144: New Ways to Heal Your Digestive Tract.
Supplying Healthy Microbes via Colonoscopy:
A team of researchers has just tested the effectiveness of supplying fecal microbiota via colonoscopy to prevent recurrent infections (Therapeutic Advances in Gastroenterology, April 22, 2025). They used a concoction of live fecal microbiota called Rebyota. The FDA approved this treatment for preventing recurrent C diff infections. It was originally designed to be administered rectally, somewhat like an enema.
The volunteers had suffered an average of three previous C diff episodes for which they had taken some powerful antibiotics. Six months after treatment with Rebyota, 95% of the participants were judged to have had successful treatment without recurrence. The side effects were primarily digestive in nature, and the treating physicians characterized them as mild.
Citations
- Jencson AL et al, "Spores on wheels: Wheelchairs are a potential vector for dissemination ofpathogens in healthcare facilities." American Journal of Infection Control, April 2019. DOI: 10.1016/j.ajic.2018.09.030
- Li X et al, "Clinical efficacy and microbiome changes following fecal microbiota transplantation in children with recurrent Clostridium difficile infection." Frontiers in Microbiology, Nov. 2, 2018. DOI: 10.3389/fmicb.2018.02622
- Khanna S et al, "Safety and effectiveness of fecal microbiota, live-jslm (REBYOTA®) administered by colonoscopy for prevention of recurrent Clostridioides difficile infection: 8-week results from CDI-SCOPE, a single-arm, phase IIIb trial." Therapeutic Advances in Gastroenterology, April 22, 2025. DOI: 10.1177/17562848251339697

