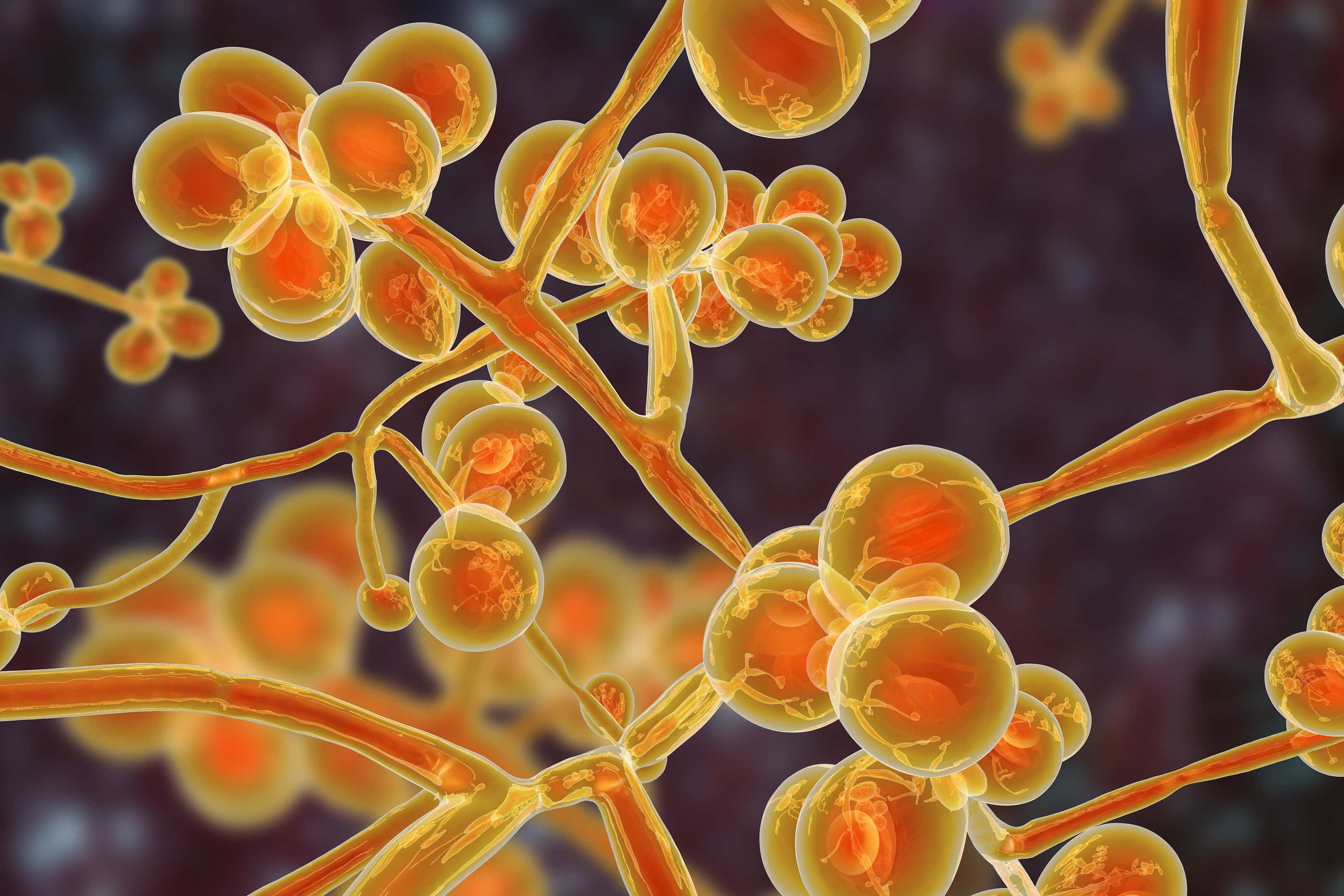
An old schoolyard refrain, “there’s a fungus among us,” once got a laugh. We are not laughing anymore! The fungus Candida auris is spreading rapidly in the US! It’s a potentially deadly fungal infection. We do not have good treatments for this threat. The fungus is becoming resistant to the drugs that we do have (echinocandins). Once this invader gets a foothold in a healthcare facility, it is extremely difficult to eradicate. A lot of hospitals and nursing homes are not revealing outbreaks.
We warned you about this potentially lethal problem back on December 25, 2019. That is when we interviewed New York Times journalist Matt Richtel on our syndicated public radio show. His article (New York Times, April 8, 2019) caught our attention. It was titled:
“Candida Auris: The Fungus Nobody Wants to Talk About”
Matt convinced us that this fungal infection was not something to ignore! That is why we talked with him. You can stream the audio by clicking on the link below or downloading the free mp3 file at this link.
Show 1192:
How a Scary Fungus Is Threatening the World
What’s Happened to Candida auris Over the Last Few Years?
It spread! We understand that scientists at the CDC and infectious disease experts around the country were preoccupied with COVID-19. But while they were focused on SARS-CoV-2, they dropped the ball on a potentially lethal fungal infection that is spreading fast!
The CDC rang the alarm bell almost a year ago (Annals of Internal Medicine, March 21, 2023). The title of this article is:
“Worsening Spread of Candida auris in the United States, 2019 to 2021″
Here were the conclusions:
“C auris cases and transmission have risen in recent years, with a dramatic increase in 2021. The rise in echinocandin-resistant cases and evidence of transmission is particularly concerning because echinocandins are first-line therapy for invasive Candida infections, including C auris. These findings highlight the need for improved detection and infection control practices to prevent spread of C auris.”
King County, Washington Has Been Invaded:
The population of King County, Washington is over 2 million. It is the most populated county in the state and includes cities such as Seattle, Bellevue, Redmond and Kirkland. Kindred Hospital in downtown Seattle is an 80-bed long-term acute care facility.
This week (Feb. 5, 2024), it was reported that Kindred had at least four cases of Candida auris infections. That may not seem like many, but once this fungus gets into a hospital it can be hard to eradicate.
Why Should You Care About Candida auris?
This fungus is not usually a threat to those who are healthy, but people with invasive medical devices or who must spend weeks in the hospital are at risk. Among such individuals, the infection has a high death rate.
More and more people have medical devices in their bodies. Pacemakers, for example, can harbor the fungus.
According to StatPearls (Feb. 19, 2023):
“Studies have found that C. auris may be found in patients’ rooms and outside the patient’s rooms in hallways, chairs, beds, windowsills, counters, electrocardiogram leads, blood pressure cuffs, infusion pumps, and ventilators. Shared multi-use patient equipment such as temperature probes and pulse oximeters may act as reservoirs of C. auris. Laboratory studies of C. auris persistence show that it may survive on moist or dry surfaces for seven days. Another study showed that C. auris cells might remain viable for up to 4 weeks and culturable for two weeks.
“Risk factors Include:
- Presence of a central venous catheter
- Indwelling urinary catheter
- Immunosuppressive state (human immunodeficiency virus, hematologic malignancy, solid tumors, transplant recipients, neutropenia, chemotherapy, corticosteroid therapy)
- Diabetes mellitus
- Chronic kidney disease
- Exposure to broad-spectrum antibiotics or previous exposure to antifungal agents within 30 days, etc.”
What Are the Symptoms of a C. auris Fungal Infection?
Readers of this article spanked me for not writing about the symptoms of a Candida auris fungal infection. That was a serious mistake on my part. But you will soon see why the answer is not as clear cut as you might like.
Here is what the CDC offers about symptoms of C. auris:
- “Symptoms may not be noticeable, because patients with C. auris infection are often already sick in the hospital with another serious illness or condition.
- Symptoms of C. auris infection depend on the part of the body affected. C. auris can cause many different types of infection, such as bloodstream infection, wound infection, and ear infection.
- Because symptoms can vary greatly, a laboratory test is needed to determine whether a patient has a C. auris infection.”
Okay, that is not very satisfactory. There’s nothing there that you can sink your teeth into, so to speak. What I am about to share is equally unsatisfying. Someone who develops a fever and chills could have this fungus, especially if the infection lingers and antibiotics do not help. That is pretty nonspecific and unhelpful.
Now you begin to understand the problem. The Cleveland Clinic describes “invasive candidiasis” this way:
Symptoms may include:
• “Belly pain.
• Chills or fever.
• Low blood pressure.
• Muscle aches.
• Skin rash.
• Weakness or fatigue.”Other symptoms to be aware of:
- Shortness of breath
- Cough
- Fatigue
- Rashes
- Headaches
There are all nonspecific symptoms. Colds, COVID or influenza can produce similar symptoms. You can see why such a fungal infection would pose a diagnostic challenge for doctors. But wait, it gets worse.
It’s hard to diagnose Candida auris. That’s because there is no easy lab test to identify this fungus. Doctors will need to perform blood cultures. It can take several days to get results and the CDC notes that C. auris may be “misidentified” as another form of Candida.
Inadequate Treatments for Candida auris:
Very few antifungal drugs are effective against C. auris. Drug resistance is becoming a huge problem in hospitals and nursing homes.
Tens of millions of people are immunocompromised. In other words, their immune system have been suppressed by medications they are taking. Once Candida auris becomes a bloodstream infection, it can cause failure of kidneys, and many other organs including brain, heart and lungs.
As noted above, spores of this yeast can linger on surfaces and may be transmitted that way or directly from person to person through contact. Eliminating the fungus from intensive care units or operating rooms can be incredibly challenging. Researchers suspect that severe strain on the healthcare system caused by the pandemic may have contributed to its spread.
The CDC warns that:
“C auris remains an ongoing health threat in the United States. Public health and health care facilities already have limited resources and IPC [infection prevention and control] capacity, and they experience further challenges with MDRO [multidrug-resistant organisms] surveillance and prevention when those limited resources shift to fight other threats, such as the COVID-19 pandemic.”
The CDC’s conclusions:
“C auris cases and transmission have risen in recent years, with a dramatic increase in 2021. The rise in echinocandin-resistant cases and evidence of transmission is particularly concerning because echinocandins are first-line therapy for invasive Candida infections, including C auris. These findings highlight the need for improved detection and infection control practices to prevent spread of C auris.”
Preventing the Spread of C. auris:
You will see that another reader asked about cleaning a hospital room if C. auris is present. Here’s another problem. Hospitals may not always let people know that this fungus is on the loose. It is not good for business.
Eradicating the fungus is challenging!
Here is what the CDC recommends. Again, not very satisfying:
“CDC recommends using an Environmental Protection Agency (EPA)–registered hospital-grade disinfectant effective against C. auris. See EPA’s List P for a current list of EPA-approved products for C. auris. If the products on List P are not accessible or otherwise suitable, facilities may use an EPA-registered hospital-grade disinfectant effective against C. difficile spores (List K) for the disinfection of C. auris. Regardless of the product selected, it is important to follow all manufacturer’s directions for use, including applying the product for the correct contact time.”
If you check out the hospital-grade disinfectants on List P, you will discover that a bleach solution and isopropyl alcohol are on the list.
Stay tuned to the People’s Pharmacy for more information about Candida Auris. We will continue to bring you updates as they unfold. In the meantime, wash hands very carefully every time you are in a healthcare facility! There is a nasty fungus among us and you do not want to bring it home.

